Amiodarone-Digoxin-Warfarin Interaction Calculator
Dose Adjustment Guide
This tool calculates appropriate dose reductions for digoxin and warfarin when starting amiodarone. These adjustments are critical to prevent life-threatening interactions.
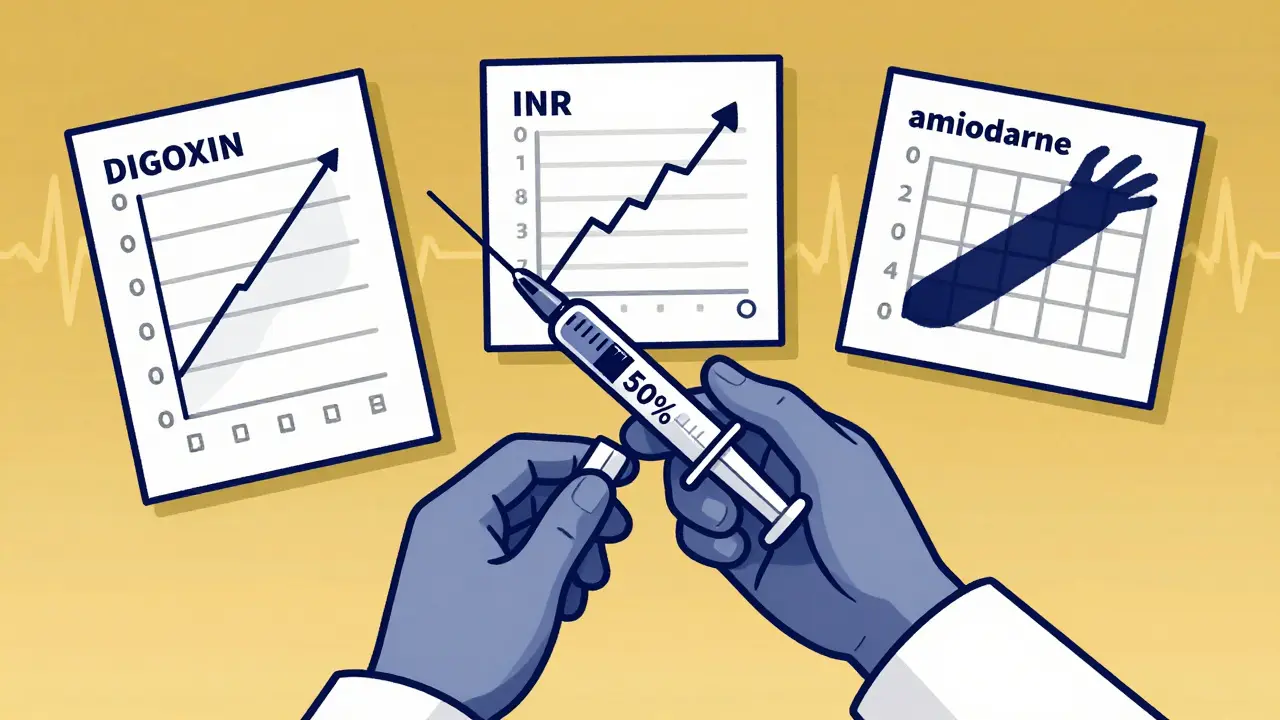
Important: Always reduce digoxin by 50% immediately when starting amiodarone. Reduce warfarin by 30-50% before or at the same time. Monitor INR closely for 4-6 weeks after stopping amiodarone due to its long half-life.
Recommended Adjustments
Digoxin Adjustment:
Warfarin Adjustment:
Critical Monitoring Schedule
- Check INR every 48-72 hours for the first 2 weeks
- Then check weekly until stable
- Continue monitoring for 4-6 weeks after stopping amiodarone
- Check digoxin levels 72 hours after starting amiodarone
Failure to follow these guidelines increases risk of toxicity by up to 23% for digoxin and 4.2x risk of INR >4.0 for warfarin.
When three common heart medications are taken together-amiodarone, digoxin, and warfarin-they don’t just coexist. They collide. And the result can be deadly.
This isn’t theoretical. It’s happening right now in hospitals and homes across the country. A 78-year-old woman with atrial fibrillation, on warfarin for stroke prevention and digoxin to control her heart rate, starts amiodarone after a scary episode of rapid heartbeat. Three days later, she’s vomiting, seeing halos around lights, and her INR spikes to 11. She ends up in the ER with internal bleeding. This scenario isn’t rare. It’s predictable. And it’s preventable-if you know what to look for.
Why This Triad Is So Dangerous
Amiodarone is a powerful antiarrhythmic. It keeps erratic heart rhythms in check, especially in atrial fibrillation. Digoxin slows the heart rate in the same condition. Warfarin thins the blood to prevent clots. Individually, each drug is manageable. Together, they amplify each other’s risks in ways most clinicians still underestimate.
The core problem? Amiodarone doesn’t just interact with one of these drugs-it hijacks the way both digoxin and warfarin are processed in the body. It blocks the pumps that clear digoxin from the kidneys and gut. It shuts down the liver enzymes that break down warfarin. The result? Digoxin levels can jump 70% within a week. Warfarin’s effect can double. And because amiodarone sticks around for months-even after you stop taking it-these changes don’t go away quickly.
This isn’t a minor adjustment. It’s a full-blown pharmacological storm. The American Heart Association estimates that over 12 million Americans have atrial fibrillation. Roughly half of them are on warfarin. A third are on digoxin. And many of those on digoxin are also on amiodarone. That’s millions of people walking around with a ticking time bomb in their bloodstream.
How Amiodarone Messes With Digoxin
Digoxin is a narrow-therapeutic-index drug. That means the difference between a therapeutic dose and a toxic one is tiny. Normal levels are between 0.5 and 0.9 ng/mL. Anything above 1.2 ng/mL in an older adult is a red flag.
When amiodarone enters the picture, it blocks a transporter called P-glycoprotein. This protein normally pushes digoxin out of kidney cells and intestinal cells so it can be cleared from the body. Without that pump working, digoxin builds up. Studies show serum levels rise by 40% to 100% within days. The effect is dose-dependent: the more amiodarone you take, the worse it gets.
Symptoms of digoxin toxicity are easy to miss. Nausea, vomiting, fatigue-people chalk it up to aging or the flu. But visual disturbances? Seeing yellow halos around lights? That’s classic. And then there’s the arrhythmias: new-onset ventricular tachycardia, bradycardia, or heart block. These aren’t side effects. They’re warning signs of imminent cardiac arrest.
One 2021 study found that patients on both amiodarone and digoxin had a 23% higher risk of death than those on digoxin alone. That’s not a small increase. That’s a clinical emergency waiting to happen.
How Amiodarone Turns Warfarin Into a Weapon
Warfarin is already a tricky drug. It interacts with food, alcohol, antibiotics, even herbal supplements. But add amiodarone, and the risk skyrockets.
Amiodarone and its metabolite, desethylamiodarone, block CYP2C9-the main enzyme that breaks down the more potent S-warfarin molecule. This cuts the clearance of S-warfarin by 55%. The result? Warfarin builds up faster than the body can handle. INR levels, which should stay between 2.0 and 3.0, can jump to 5, 8, even 12 in a matter of days.
And it’s not just the numbers. High INR means bleeding. Major bleeding happens in 12-18% of patients on warfarin when this interaction isn’t managed. Intracranial hemorrhage? That’s the nightmare scenario. The FDA reported 387 deaths in 2022 alone linked to this triad. That’s not an outlier. That’s a pattern.
What makes it worse? Digoxin can also displace warfarin from protein-binding sites in the blood. So now you’ve got two mechanisms pushing warfarin levels higher-amiodarone slowing its breakdown, and digoxin pushing more of it into circulation. It’s a double hit.
What Happens When You Don’t Adjust Doses
Here’s what too many providers do: they start amiodarone and assume the other meds are fine. They don’t change the digoxin dose. They don’t check the INR for a week. That’s how patients end up in the ICU.
A 2020 study of over 12,000 patients on warfarin found that those taking amiodarone were 4.2 times more likely to have an INR over 4.0. They were nearly three times more likely to suffer major bleeding. In one case documented by a cardiologist on Reddit, a patient’s INR hit 12.4 after just 10 days on amiodarone. He needed four units of fresh frozen plasma and IV vitamin K to survive.
And the risk doesn’t disappear when you stop amiodarone. Because amiodarone has a half-life of 25 to 100 days, its effects linger. A patient might stop amiodarone on a Monday, and by Friday, their INR is still climbing. That’s why guidelines say to keep monitoring for 4 to 6 weeks after discontinuation.
How to Manage This Triad Safely
There’s no magic bullet. But there is a proven protocol. And it’s simple-if you follow it.
- Reduce digoxin by 50% immediately when starting amiodarone. Don’t wait. Don’t monitor first. Start low.
- Check serum digoxin levels 72 hours after starting amiodarone. If it’s above 1.2 ng/mL, cut the dose again.
- Reduce warfarin by 30-50% before or at the same time as starting amiodarone. This isn’t optional. It’s mandatory.
- Check INR every 48-72 hours for the first two weeks. Then weekly until stable. Don’t rely on a single value-look at the trend.
- Keep monitoring for 4-6 weeks after stopping amiodarone. The drug is still in the system. The risk isn’t gone.
These steps aren’t suggestions. They’re survival tactics. A 2023 NHS England report showed that hospitals that enforced this protocol reduced adverse events by 78% in just one year.
What About Newer Anticoagulants?
Many patients today are switched from warfarin to DOACs-drugs like apixaban, rivaroxaban, or dabigatran. These don’t need regular INR checks and have fewer food interactions.
But here’s the catch: amiodarone still affects them. It inhibits P-glycoprotein, which is how dabigatran is cleared. Studies show dabigatran levels can rise by 50-100% when taken with amiodarone. The FDA now warns against combining dabigatran with amiodarone in patients over 75.
So switching from warfarin to a DOAC doesn’t eliminate the risk-it just changes the shape of it. You still need to reduce digoxin. You still need to monitor closely. And you still need to know that amiodarone doesn’t play nice with anything.
Who’s at Highest Risk?
This isn’t a young person’s problem. The average patient in these dangerous combinations is over 75. They often have kidney issues, which slows drug clearance even more. They’re on multiple meds-statins, diuretics, beta-blockers. Their bodies can’t handle the extra burden.
Studies show that 63% of adverse events involving this triad occur in patients over 75. Many of them have fallen, hit their head, and ended up with intracranial bleeding because their INR was sky-high and no one checked it.
It’s also more common in patients with mechanical heart valves. They can’t use DOACs. They’re stuck on warfarin. And if they have persistent atrial fibrillation, they’re likely on amiodarone and digoxin too. That’s the perfect storm.
What Clinicians Need to Do Differently
Electronic health records should flag this combination automatically. But too many systems don’t. Or they flag it too late-after the patient is already on all three drugs.
Every time you’re about to prescribe amiodarone, ask: Is the patient on digoxin? Are they on warfarin? If yes, you don’t just add a new drug. You reset the whole plan.
Don’t assume the pharmacist caught it. Don’t assume the patient remembers their meds. Don’t assume the INR was checked last week. Do the math. Do the checks. Document everything.
As Dr. William J. Mandel, one of the original researchers on this interaction, said: “Failure to anticipate and adjust for this interaction represents one of the most preventable causes of iatrogenic harm in cardiac pharmacotherapy.” That’s not a quote. It’s a warning.
The Bottom Line
Amiodarone, digoxin, and warfarin together aren’t just a risky combo. They’re a clinical trap. And too many people fall into it because it’s so common, it feels normal.
But normal doesn’t mean safe. It means deadly.
If you’re managing a patient on this triad, you have one job: adjust doses before the drugs start working. Monitor like your life depends on it-because someone’s life does. Check digoxin levels. Check INR every few days. Reduce, don’t guess. And never assume the problem is gone after stopping amiodarone.
This isn’t about being careful. It’s about being exact. Because in this triad, there’s no room for error.
Can I still use warfarin if I need amiodarone?
Yes, but only with strict precautions. You must reduce the warfarin dose by 30-50% before or at the same time as starting amiodarone. INR must be checked every 48-72 hours for the first two weeks, then weekly. Monitoring must continue for 4-6 weeks after amiodarone is stopped because it stays in the body for months.
What happens if I don’t reduce digoxin when starting amiodarone?
Digoxin levels can rise by 70% or more within a week, leading to toxicity. Symptoms include nausea, vomiting, visual changes (yellow halos), confusion, and dangerous heart rhythms like ventricular tachycardia. In elderly patients, this can cause sudden cardiac arrest. The risk of death increases by 23% when digoxin isn’t adjusted.
Are newer anticoagulants (DOACs) safer with amiodarone?
Not necessarily. Amiodarone inhibits P-glycoprotein, which clears drugs like dabigatran. This can raise dabigatran levels by 50-100%, increasing bleeding risk. The FDA advises against combining dabigatran with amiodarone in patients over 75. DOACs reduce some risks of warfarin, but not this specific interaction.
How long does the interaction last after stopping amiodarone?
Amiodarone has an extremely long half-life-25 to 100 days. Its effects on digoxin and warfarin can persist for weeks to months after discontinuation. INR and digoxin levels must be monitored for at least 4-6 weeks after stopping amiodarone, even if the patient feels fine.
Is this interaction more dangerous in older adults?
Yes. Older adults are more vulnerable because they often have reduced kidney function, lower body weight, and take multiple medications. Studies show 63% of serious adverse events from this triad occur in patients over 75. Digoxin toxicity and major bleeding are far more likely-and more deadly-in this group.

Comments (12)