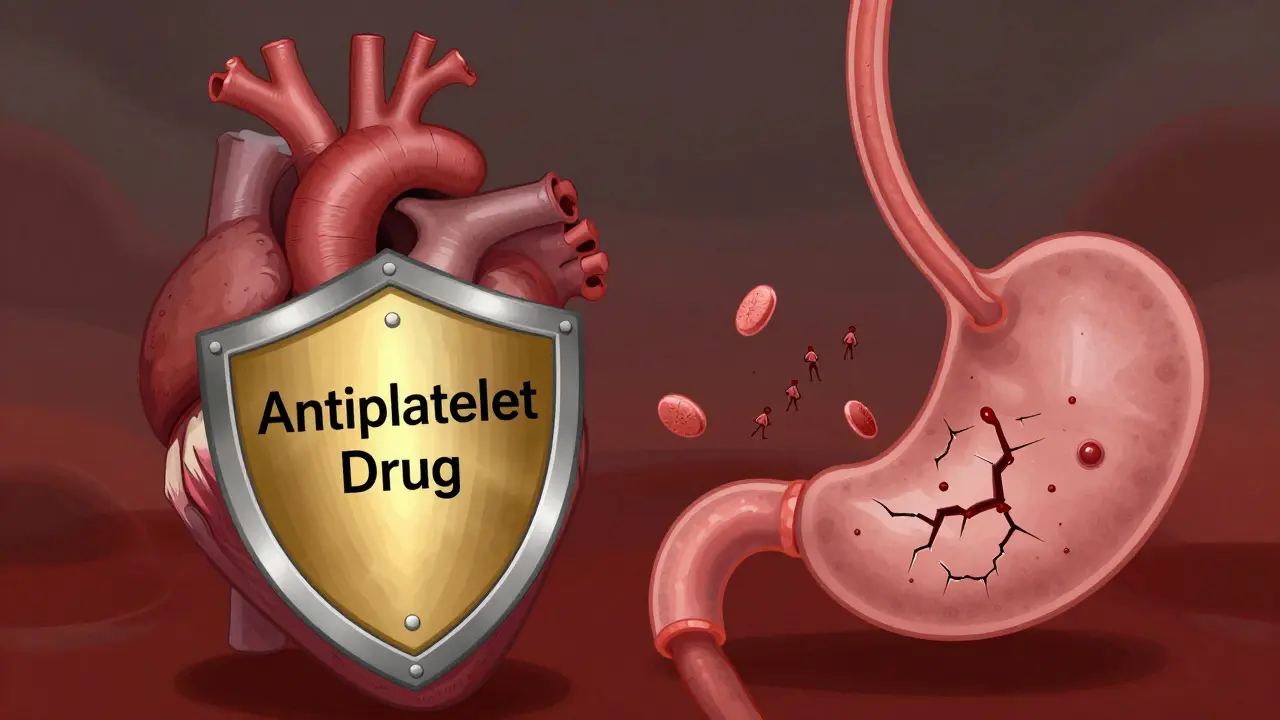
When you take an antiplatelet drug like aspirin, clopidogrel, or ticagrelor, you're not just preventing a heart attack or stroke-you're also quietly increasing your risk of bleeding, especially in your stomach. It’s a trade-off millions of people make every day, often without realizing how real the danger is. About 1 in 100 people will have noticeable gastrointestinal bleeding within the first month of starting these medications, and for those with prior ulcers, diabetes, or who are over 65, the risk jumps even higher. The good news? You don’t have to choose between protecting your heart and protecting your stomach. There are clear, proven ways to reduce the damage-without giving up the life-saving benefits.
How Antiplatelet Drugs Work (and Why They Hurt Your Stomach)
Antiplatelet medications stop your blood platelets from clumping together. That’s how they prevent dangerous clots from forming in your arteries after a heart attack, stent placement, or stroke. But platelets aren’t just involved in clotting-they also help repair tiny tears in your stomach lining. When you block them, your stomach loses its natural healing shield.
Aspirin is the oldest and most widely used. It works by permanently disabling the COX-1 enzyme, which reduces both inflammation and platelet activity. Even enteric-coated aspirin-designed to dissolve in the intestine instead of the stomach-doesn’t stop the systemic effect. The drug still gets into your bloodstream and suppresses platelets everywhere, including your gut.
The newer drugs-clopidogrel, prasugrel, and ticagrelor-block a different pathway called P2Y12. They’re stronger at preventing clots, which is why they’re often used after stents. But they’re also harder on the stomach. Studies show clopidogrel causes more gastric injury than aspirin, with a hazard ratio of 1.8. Prasugrel and ticagrelor are even worse: ticagrelor increases GI bleeding risk by 30% compared to clopidogrel. Why? These drugs don’t just stop clotting-they interfere with the growth factors your stomach needs to repair ulcers.
The Real Risk: Who’s Most Likely to Bleed?
Not everyone on antiplatelets will bleed. But certain factors make it much more likely:
- Age 65 or older
- History of peptic ulcer or GI bleeding
- Taking NSAIDs like ibuprofen or naproxen at the same time
- Infection with H. pylori bacteria
- Using blood thinners like warfarin or apixaban alongside
- On dual antiplatelet therapy (DAPT)-aspirin plus clopidogrel or ticagrelor
DAPT raises your bleeding risk by 30-50% compared to just one drug. And here’s the catch: many people don’t realize they’re on DAPT. After a heart attack or stent, doctors often prescribe both for 6-12 months. But if you’ve had a bleed before, staying on both may not be worth it.
A 2023 study of over 4,800 patients after stent placement found that 1% had overt GI bleeding within 30 days. But among those with prior ulcers, the rate was closer to 8%. And after 6-12 months of continuous use, up to 50% of clopidogrel users show signs of progressive stomach damage-even if they feel fine.
Protecting Your Stomach: The Proven Solution
If you’re on antiplatelet therapy and have any risk factors, you need a stomach protector. And the only proven, guideline-backed option is a proton pump inhibitor (PPI).
PPIs like esomeprazole (Nexium), omeprazole (Prilosec), and pantoprazole (Protonix) shut down acid production in your stomach. Less acid means less irritation, and more time for your stomach lining to heal-even with platelets suppressed.
Guidelines from the American College of Gastroenterology and Canadian Association of Gastroenterology (2023) are clear: if you’ve had a previous ulcer or GI bleed, take a PPI for at least 8 weeks after healing-and often for life. For high-risk patients, esomeprazole 40mg daily is the gold standard. One study showed 92% of patients with ulcers on clopidogrel had complete healing in just 8 weeks when given esomeprazole.
And here’s something many don’t know: you should keep taking your PPI even if you’ve had a bleed. Stopping it doesn’t reduce rebleeding-it increases it.
What About the Clopidogrel-PPI Interaction?
You’ve probably heard that PPIs can reduce clopidogrel’s effectiveness. It’s true-some PPIs interfere with how clopidogrel is activated in the liver. But here’s the reality: the clinical impact is small and often overstated.
The FDA looked into this in 2010 and said the evidence was uncertain. Later studies found a 20-30% higher risk of heart attacks or stent clots in patients taking both, but those were mostly observational and didn’t prove cause and effect. More recent, larger studies show no meaningful increase in cardiovascular events when using PPIs with clopidogrel.
Still, if you’re worried, there’s a simple fix: take your PPI in the evening and your clopidogrel in the morning. This separates the timing enough to reduce any potential interaction. Omeprazole and esomeprazole have the strongest interaction, so if you’re on clopidogrel, pantoprazole or dexlansoprazole are safer choices.
And remember: if you’re on aspirin alone, PPIs don’t interfere at all. Aspirin doesn’t rely on liver activation like clopidogrel does.
What to Do If You Bleed
If you notice black, tarry stools, vomiting blood, or sudden dizziness and weakness, get help immediately. Don’t wait. But here’s what you shouldn’t do: stop your antiplatelet medication without talking to your doctor.
Stopping aspirin during a GI bleed increases your risk of death by 25%, according to a landmark 2017 Lancet study. The same study found that continuing aspirin didn’t worsen bleeding-it actually improved survival. That’s because the clotting risk from stopping the drug outweighs the bleeding risk.
For P2Y12 inhibitors like clopidogrel or ticagrelor, guidelines say to pause them for 5-7 days during active bleeding. But restart them as soon as your doctor says it’s safe. Delaying too long can lead to stent thrombosis-where a clot forms inside your stent, causing a heart attack.
And don’t let anyone give you a platelet transfusion. Studies show patients who get platelet transfusions during GI bleeding have a 27% death rate-compared to 12% for those who don’t. The transfused platelets can worsen clotting in the wrong places and increase pressure in bleeding vessels.
What About Other Options? H2 Blockers, Sucralfate, or Natural Remedies?
H2 blockers like famotidine (Pepcid) or ranitidine (Zantac) reduce acid, but they’re not strong enough to protect against antiplatelet-induced ulcers. Studies show they’re less effective than PPIs by a wide margin.
Sucralfate forms a protective coating, but it doesn’t reduce acid. It’s useful for short-term healing, but not for long-term prevention.
And no, ginger, aloe vera, or probiotics won’t stop this kind of bleeding. They might help with general digestion, but they don’t replace the biological protection PPIs provide. Don’t gamble with your heart or your stomach.
When to Consider Switching Medications
If you’ve had multiple GI bleeds despite taking a PPI, your doctor might consider switching your antiplatelet drug. Aspirin monotherapy is the safest option for long-term use after a bleed. It’s cheaper, has less GI risk than clopidogrel, and doesn’t interact with PPIs.
Prasugrel and ticagrelor are powerful, but their bleeding risk makes them poor choices for people with a history of ulcers. If you’re on one of these and keep having stomach problems, ask if you can switch to aspirin plus a PPI. You’ll lose a bit of clot protection-but gain much more safety.
And if you’re a clopidogrel non-responder (due to a CYP2C19 gene variant), you might benefit from switching to ticagrelor or prasugrel for better heart protection-but only if you’re also on a PPI and have no history of GI issues.

What’s Next? The Future of Safer Antiplatelets
Researchers are working on drugs that block platelets in the arteries but leave stomach platelets alone. One promising candidate, selatogrel, is in Phase III trials and shows 35% less stomach damage than ticagrelor in early studies. It’s not available yet, but it’s a sign that the field is moving toward smarter, safer options.
Another big shift is coming: personalized medicine. Blood tests for pepsinogen and gastrin-17 levels may soon help predict who’s at highest risk for GI bleeding before it happens. Within five years, your doctor might use a simple blood test to decide whether you need a PPI, a different drug, or both.
For now, the best strategy is simple: know your risk, take your PPI if you need it, and never stop your antiplatelet without talking to your doctor.
Frequently Asked Questions
Can I take ibuprofen with aspirin or clopidogrel?
No. Taking NSAIDs like ibuprofen, naproxen, or diclofenac with antiplatelet drugs doubles your risk of GI bleeding. Even occasional use is dangerous. If you need pain relief, use acetaminophen (Tylenol) instead. It doesn’t affect platelets or the stomach lining.
Is it safe to take a PPI long-term?
Yes, for most people. Long-term PPI use is safe when medically necessary. Some people worry about bone loss or kidney issues, but these risks are very low and mostly seen in people taking high doses for over 10 years. For patients on antiplatelets with a history of bleeding, the benefits far outweigh the risks. Your doctor should review your need for PPIs annually.
I feel fine-do I still need a PPI?
If you have risk factors-age over 65, past ulcer, H. pylori, or on DAPT-then yes. GI damage from antiplatelets often happens without symptoms. By the time you feel pain, bleeding may already be underway. Preventive PPI use is like wearing a seatbelt: you don’t wait for a crash to use it.
Can I stop my antiplatelet drug if I’m worried about bleeding?
Never stop without talking to your cardiologist. Stopping aspirin or clopidogrel suddenly increases your risk of heart attack or stroke by up to 50% in the first month. If you’re scared, talk to your doctor about switching to a safer option like aspirin plus a PPI. Don’t quit cold turkey.
What if I can’t tolerate PPIs?
About 15-20% of people have side effects like diarrhea, headaches, or nausea with PPIs. If you can’t take them, ask about switching to aspirin monotherapy, which has lower GI risk. Your doctor might also consider a different PPI like dexlansoprazole, which is better tolerated. In rare cases, misoprostol can be used, but it’s not ideal due to side effects like cramping.
What to Do Next
If you’re on an antiplatelet drug:
- Ask your doctor if you’re at risk for GI bleeding. Use the AIMS65 score: Age ≥65, INR >1.5, Albumin <3.0, Mental status change, Systolic BP ≤90.
- If you have any risk factors, ask for a PPI. Don’t wait for symptoms.
- Stop NSAIDs. Switch to acetaminophen for pain.
- If you’ve had a bleed before, ask if you can switch from clopidogrel or ticagrelor to aspirin alone.
- Never stop your antiplatelet drug without medical advice.
Your heart needs protection. So does your stomach. With the right strategy, you can keep both safe.
Comments (8)