When you hear the word breast cancer, what comes to mind? Fear? Uncertainty? Maybe both. But here’s the truth: early detection saves lives. And the most proven tool we have for catching it early isn’t a fancy lab test or a genetic scan-it’s a simple, widely available imaging test called mammography. In 2026, the rules around who should get screened, when, and how have changed. They’re clearer. More consistent. And they’re designed to catch cancer before it spreads.
Who Should Be Screened, and When?
For years, women were told to start mammograms at 50. Then 45. Then some were told to wait until they felt a lump. But the data doesn’t support waiting. In South Africa, as in the U.S., more women under 50 are being diagnosed with invasive breast cancer than ever before. That’s why nearly all major medical groups now agree: screening should start at age 40. The American College of Obstetricians and Gynecologists updated its guidelines in October 2024 to say all women at average risk should begin annual mammograms at 40. The U.S. Preventive Services Task Force still recommends biennial screening for women 40 to 74, but they now give a Grade B recommendation for women in their 40s-meaning the benefit is clear enough to encourage it, not just suggest it. The American Cancer Society lets women 40 to 44 choose whether to start, but strongly recommends annual screening from 45 to 54. After 55, you can switch to every two years-or keep going yearly if you prefer. The American Society of Breast Surgeons takes the strongest stance: start at 40, continue yearly until your life expectancy drops below 10 years. Why? Because early-stage breast cancer, when caught before it spreads to lymph nodes, has a 99% five-year survival rate. Waiting until 50 means missing years where cancer can grow unnoticed.2D vs. 3D Mammography: What’s the Difference?
Most women still get 2D mammograms. That’s the traditional X-ray image of the breast from two angles. But now, digital breast tomosynthesis-also called 3D mammography-is becoming the new standard. Instead of one flat image, 3D mammography takes dozens of thin slices through the breast, like flipping through pages of a book. This helps doctors see through overlapping tissue, which is especially helpful for women with dense breasts. Dense breasts aren’t rare. About half of all women have them. And in dense tissue, cancers can hide in 2D images. Studies show 3D mammography finds 40% more invasive cancers than 2D alone and reduces false positives by up to 15%. That means fewer unnecessary callbacks for extra tests. The American Society of Breast Surgeons recommends 3D mammography as the preferred screening method. Medicare covers one baseline mammogram in your lifetime and annual screening mammograms. Most private insurers now cover 3D mammography as part of routine screening. If your facility offers it, ask for it. If they don’t, ask why.What About Women at Higher Risk?
If you have a family history of breast cancer, a BRCA1 or BRCA2 mutation, or had radiation to your chest before age 30, your risk is higher. So is your need for more than just a mammogram. The American Cancer Society recommends annual mammograms plus breast MRI for women with a lifetime risk of 20% to 25% or higher. That’s calculated using tools like Tyrer-Cuzick or BOADICEA, which look at family history, age at first period, number of children, and other factors. These tools are now part of routine care at many clinics. MRI is more sensitive than mammography, but it’s also more likely to show something that turns out to be harmless. That’s why it’s only recommended for high-risk women-not everyone with dense breasts. For women with dense breasts but no other risk factors, the USPSTF says there’s not enough proof to recommend ultrasound or MRI as routine additions. Still, if you’re worried, talk to your doctor. Some clinics offer supplemental screening on a case-by-case basis.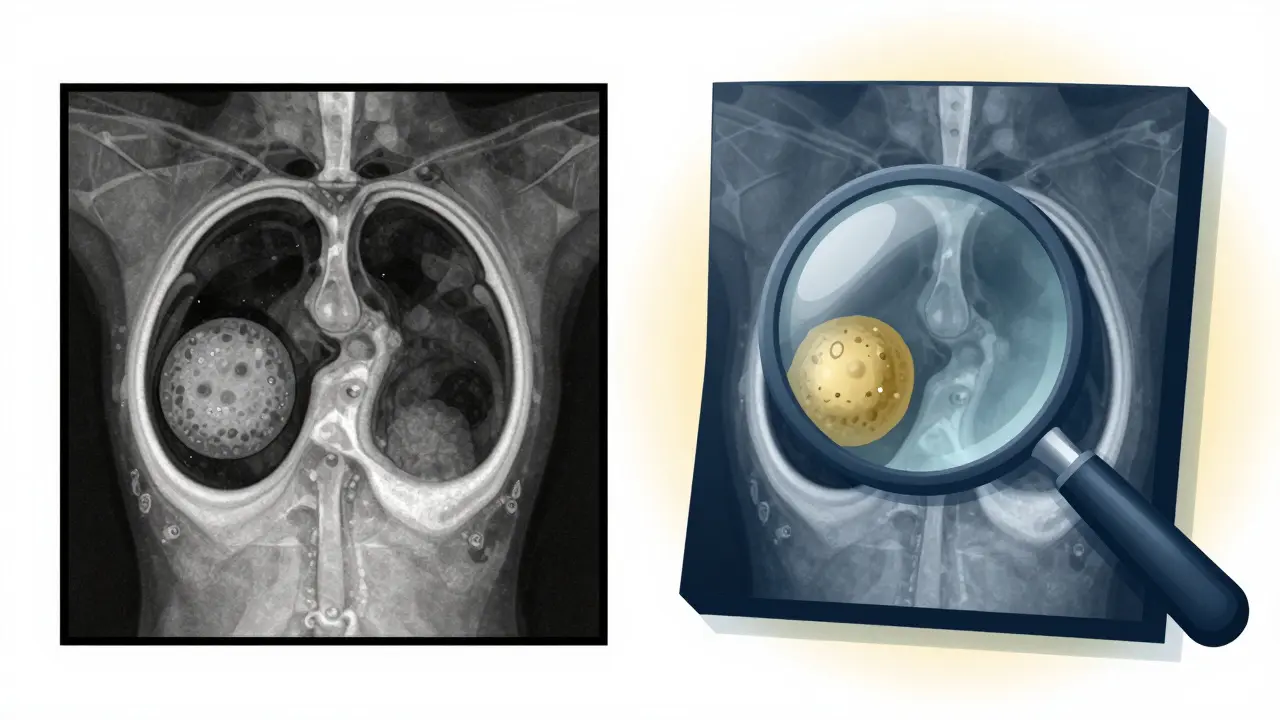
How Effective Is Screening Really?
Let’s talk numbers. A major analysis of nine clinical trials found that regular mammography reduces the risk of dying from breast cancer by about 12%. That might sound small, but it’s the same as preventing one death for every 1,000 women screened over 10 years. And that’s just for women aged 40 to 74. The real win isn’t just in survival rates-it’s in treatment. When cancer is caught early, you’re more likely to need less aggressive treatment. Early-stage tumors often mean lumpectomy instead of mastectomy. No chemotherapy. No radiation. Or just a few weeks of it. Late-stage cancer? That’s often full chemotherapy, multiple surgeries, and years of hormone therapy. The shift to starting at 40 isn’t just about statistics. It’s about equity. Black women in the U.S. and South Africa are more likely to die from breast cancer. Why? Often, they’re diagnosed later. Starting screening at 40 helps close that gap.What Happens After a Diagnosis?
Screening finds cancer. Treatment decides what happens next. But here’s the thing: there’s no one-size-fits-all plan. Treatment depends on three things: the cancer’s stage (how big it is and if it’s spread), its biology (hormone receptors, HER2 status), and you. Stage I or II cancers? Surgery is almost always the first step. That could mean removing just the tumor (lumpectomy) or the whole breast (mastectomy). Radiation usually follows lumpectomy. For some older women with slow-growing tumors, radiation might be skipped. Hormone receptor-positive cancers (the most common type) are treated with pills like tamoxifen or aromatase inhibitors for five to ten years. HER2-positive cancers get targeted drugs like trastuzumab. Triple-negative cancers-aggressive and hormone-free-often need chemotherapy. Genomic tests like Oncotype DX or MammaPrint help decide if chemotherapy will actually help. If your tumor score is low, chemo might do more harm than good. That’s huge. It means fewer women get blasted with drugs they don’t need. Sentinel lymph node biopsy is now standard. Instead of removing all underarm nodes, surgeons remove just the first one or two that drain from the tumor. If they’re clean, you avoid lymphedema and nerve damage.What About the Future?
Newer tools are coming. AI-assisted mammography is already in use in some hospitals-it helps radiologists spot subtle changes that humans might miss. Liquid biopsies, which detect cancer DNA in blood, are still experimental but show promise for monitoring recurrence. But the biggest change isn’t tech. It’s mindset. Breast cancer screening isn’t optional. It’s as routine as a dental checkup or a blood pressure test. You don’t wait for symptoms. You don’t skip it because you’re busy. You don’t avoid it because you’re scared. If you’re 40 or older, make your next appointment. If you’re under 40 and have a family history, talk to your doctor about risk assessment. If you’ve had cancer before, stay on schedule. And if you’re unsure where to start, ask your clinic if they offer risk evaluation and 3D mammography.
What If I Don’t Have Insurance?
In South Africa, public hospitals offer free mammograms for women over 40 through the National Department of Health’s breast cancer screening program. Private clinics often have sliding scale fees. Nonprofits like Breast Care SA and the National Cancer Control Programme provide free or low-cost screenings in underserved areas. You don’t need a referral. You don’t need to be a citizen. If you’re a woman over 40, you qualify.What If I’m Afraid of the Results?
That fear is real. I’ve talked to women who avoided screening for years because they didn’t want to know. But here’s what they all say after they go: "I wish I’d done it sooner." A false positive happens. A callback for extra images happens. But most of those turn out to be nothing. And if something is found? Early means easier. Less pain. Less cost. More life.What’s the Bottom Line?
Breast cancer screening isn’t perfect. But it’s the best tool we have. Starting at 40, using 3D mammography when possible, and continuing as long as you’re healthy-those are the rules that save lives. And if you’re at higher risk? Don’t wait. Get evaluated. Get the extra tests. Your future self will thank you.When should I start getting mammograms?
Most major medical organizations now recommend starting annual mammograms at age 40, even if you have no symptoms or family history. Some groups, like the U.S. Preventive Services Task Force, say biennial screening is fine for women 40 to 74, but the trend is moving toward starting at 40 and screening yearly-especially because breast cancer is rising in younger women. If you’re at higher risk due to genetics or dense breasts, you may need to start even earlier, often at 30.
Is 3D mammography better than 2D?
Yes, for most women. 3D mammography (digital breast tomosynthesis) finds more invasive cancers and reduces false alarms by 15% compared to 2D. It’s especially helpful for women with dense breasts, where tumors can hide in traditional images. While 2D is still widely used, many clinics now offer 3D as the standard. Ask if it’s available and covered by your insurance.
Do I need an MRI in addition to a mammogram?
Only if you’re at high risk-like having a BRCA mutation, a strong family history, or a lifetime risk of 20% or higher. For average-risk women, even with dense breasts, MRI isn’t routinely recommended because it leads to too many false positives. But if your doctor says you’re high risk, adding annual MRI to your mammogram can catch cancers earlier.
How often should I get screened after age 55?
You can switch to every two years if you prefer, but you don’t have to. Many women continue yearly screening because it gives them peace of mind and catches cancers earlier. The key is to keep going as long as you’re in good health and your life expectancy is over 10 years. Stopping at 65 or 70 isn’t necessary if you’re healthy.
What if I can’t afford a mammogram?
In South Africa, public hospitals offer free mammograms for women over 40 through government programs. Nonprofits like Breast Care SA and the National Cancer Control Programme also provide free or low-cost screenings in townships and rural areas. No referral is needed. You just show up. Don’t let cost stop you-early detection is free if you know where to go.
Can lifestyle changes reduce my risk?
Yes, but not enough to replace screening. Maintaining a healthy weight, limiting alcohol, exercising regularly, and avoiding hormone replacement therapy after menopause can lower your risk. But even women who live perfectly healthy lives can get breast cancer. That’s why screening isn’t optional-it’s your safety net.
Is breast self-exam still recommended?
No major organization recommends routine breast self-exams as a screening tool. Studies show they don’t reduce deaths and can lead to unnecessary anxiety and biopsies. Instead, know what’s normal for your body. If you notice a new lump, nipple discharge, skin dimpling, or persistent pain, see your doctor right away. Don’t wait for your next mammogram.

Comments (8)