Going out to eat doesn’t have to mean giving up control over your blood sugar. With diabetes, dining at a restaurant can feel like walking through a minefield of hidden sugars, oversized portions, and confusing labels. But it doesn’t have to be that way. Many people with diabetes manage to enjoy meals out regularly-without spikes, crashes, or guilt. The secret isn’t avoiding restaurants. It’s knowing how to navigate them.
Use the Plate Method-No Calculator Needed
You don’t need to count every gram of carb to eat well at a restaurant. The Diabetes Plate Method works because it’s visual, simple, and works across every type of cuisine. Grab a standard nine-inch plate. Fill half of it with non-starchy vegetables: broccoli, spinach, green beans, peppers, zucchini, or a side salad. That’s your foundation. Then, divide the other half: one quarter for lean protein (grilled chicken, fish, tofu, lean beef), and the last quarter for carbs-rice, pasta, potatoes, bread, or corn. That’s it. No math. No apps. Just a plate. Most restaurants serve portions that are two to three times larger than what you actually need. By using this method, you automatically cut down on carbs and calories without having to ask for anything special. Even if the server brings a huge plate of pasta, you mentally divide it and only eat the quarter meant for carbs. The rest? Leave it or box it before you start.Watch Out for the Hidden Carbs
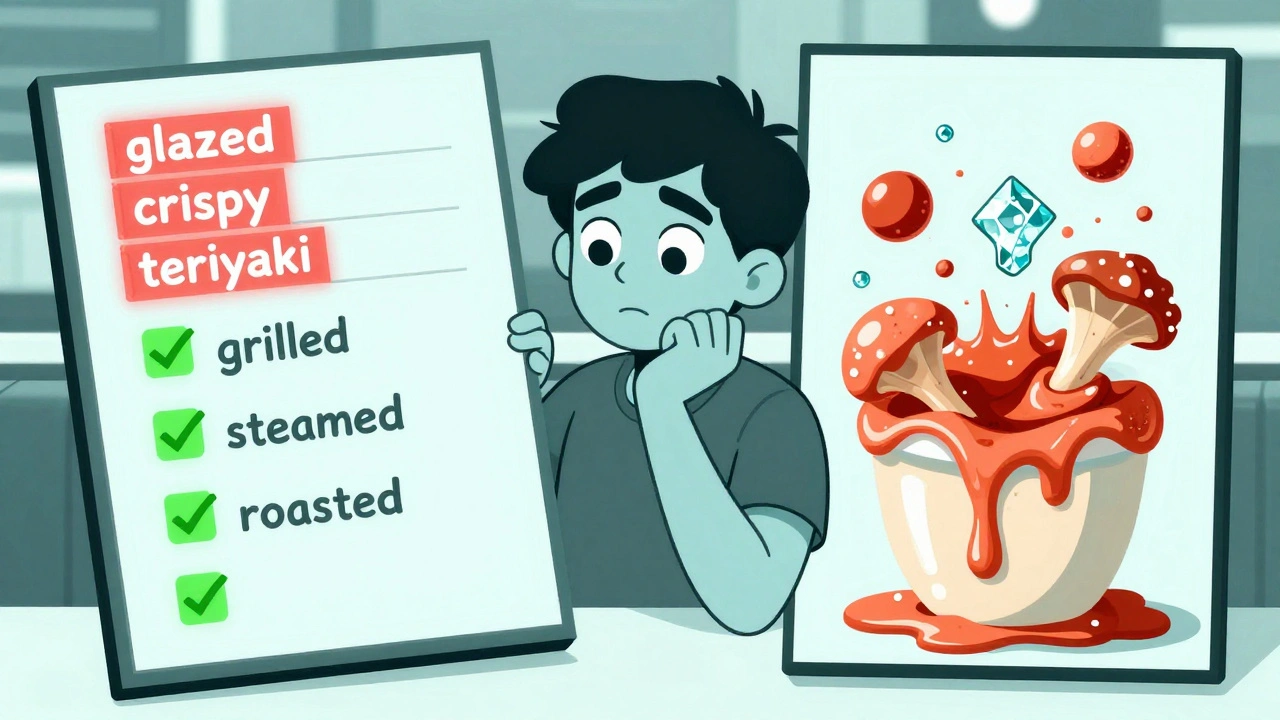
The biggest trap isn’t the obvious stuff like bread or fries. It’s the sauces, glazes, and dressings you barely notice. A tablespoon of teriyaki sauce? That’s 8 grams of carbs. Creamy mushroom sauce? Another 6-10 grams. Honey-glazed salmon? You’re looking at 15 grams of sugar before you even touch the fish. Gravies, marinades, and even "light" salad dressings often hide sugar, corn syrup, or starch. Always ask: "Can I get the sauce or dressing on the side?" Then use no more than two tablespoons. Skip anything labeled "crispy," "breaded," "au gratin," or "creamed." These words mean extra flour, breadcrumbs, or cream-each adding 10-15 grams of carbs. Instead, go for grilled, baked, steamed, or roasted. Ask for vegetables instead of fries or mashed potatoes. Most places will swap them for free.Portion Control Is Non-Negotiable
Restaurant portions are designed to overwhelm. A typical chicken entrée might come with 12 ounces of meat and a full cup of rice. That’s two full meals. You don’t need that. Here’s what works:- Order an appetizer as your main. A grilled shrimp salad or vegetable stir-fry is often enough.
- Share your meal. Split an entrée with someone. You get variety, they get company, and you both eat less.
- Ask for a half portion. Many full-service restaurants will cut a portion in half for you-sometimes even for free.
- Box half your meal before you start eating. Seriously. Do it the second the food arrives. It removes the temptation to finish everything on the plate.
Know the Red Flags on Menus
Some menu words are sugar bombs in disguise:- "Glazed" - Think honey-glazed carrots or glazed ham. Adds 10-20g carbs.
- "Crispy" - Usually breaded. Adds 15g+ carbs from flour or breading.
- "Au gratin" - Cream, cheese, and breadcrumbs. Easily 25g+ carbs.
- "Teriyaki," "sweet and sour," "hoisin" - These sauces are mostly sugar. Ask for low-sugar versions or skip them.
- "Fried" - Even "lightly fried" means batter. Avoid.
Plan Ahead-It’s the Game Changer
The most successful people with diabetes don’t wing it at restaurants. They check menus online before they leave the house. Most chains now list nutrition info, including carbs. Even if it’s not perfect, it gives you a baseline. Research from Parkview Health shows that people who review menus ahead of time are 58% more likely to stick to their carb goals. You can even call ahead and ask if they can modify dishes. Most kitchens are happy to accommodate. If you’re going somewhere new, pick a dish you know you can eat. Don’t try to be adventurous on a night when your blood sugar is already shaky. Stick to what works. Consistency beats novelty.Bring Backup-Just in Case
Restaurant service can be slow. You might wait 45 minutes for your food. If you take insulin, that delay can drop your blood sugar dangerously low. Always carry fast-acting glucose with you: glucose tablets, juice boxes, or even a few pieces of hard candy. The American Diabetes Association reports that 23% of people with diabetes have had a low blood sugar episode while dining out. That’s not rare. It’s predictable. Carry at least 15 grams of carbs. And don’t be embarrassed to check your blood sugar at the table. It’s not rude-it’s smart.Don’t Fall for "Healthy" Traps
Just because something sounds good doesn’t mean it’s low-carb. Chicken parmesan? It’s breaded, smothered in sauce, and served with pasta. That’s 65 grams of carbs-more than a whole bagel. A "salad" with grilled chicken? If it’s got croutons, dried cranberries, and ranch dressing, you’re looking at 40+ grams of carbs. Ask for details. "What’s in the dressing?" "Is the chicken breaded?" "Do you use sugar in the marinade?" Most servers can answer or find out. If they can’t, treat it like a red flag.
What About Alcohol?
Alcohol can be tricky. Beer and sweet cocktails are loaded with carbs. A 12-ounce beer has 13-20g carbs. A margarita? 25g or more. Wine is better-about 3-4g per 5-ounce glass. Stick to dry wines, light beer, or spirits with soda water and lime. No sugary mixers. Also, alcohol can mask the symptoms of low blood sugar. You might feel dizzy or shaky and think it’s just the drink. Always check your blood sugar before drinking and eat something with protein or fat at the same time.It Gets Easier
The first few times you try to eat out with diabetes, it feels awkward. You’re asking for substitutions, boxing food, checking labels. You might feel like you’re the only one doing it. But you’re not. And it gets easier. After three or four successful outings, you start recognizing patterns. You learn which restaurants are easiest. You know which dishes to avoid. You get comfortable saying, "I need to keep my carbs low. Can you help me?" Most people are happy to help. Servers want you to enjoy your meal. And the more you do it, the more restaurants start noticing. In 2024, 20 major chains rolled out a "Dine Smart" symbol on menus to flag meals with 45 grams of carbs or less. That’s progress.Carbs Aren’t the Enemy-Mismanagement Is
You don’t need to eliminate carbs. You need to manage them. A small portion of whole grains, beans, or fruit can fit into your plan. The goal isn’t perfection. It’s consistency. One meal with 70g of carbs won’t ruin your health. But doing it every night? That’s a problem. Focus on balance. Protein + veggies + controlled carbs. That’s your formula. And it works whether you’re at a taco truck, a sushi bar, or a steakhouse.What If You Overdo It?
You ordered the pasta. You ate the bread. You had dessert. It happens. Don’t panic. Don’t skip your insulin or punish yourself. Just move on. Check your blood sugar. If it’s high, take your correction dose if your doctor told you to. Drink water. Go for a walk after eating. Your body will handle it better than you think. The key is not to let one meal derail your next one. Diabetes management is a long game. One bad meal doesn’t define you. But how you respond to it? That does.Can I still eat at fast-food places with diabetes?
Yes, but you need to be selective. Skip the burgers with buns and fries. Opt for grilled chicken sandwiches without the bun, or a side salad with grilled chicken and vinaigrette on the side. A plain grilled chicken wrap without sauce has about 20g carbs. A Big Mac? 46g. Choose wisely. Many chains now list carb counts online-use them.
Do I need to count carbs every time I eat out?
Not if you use the plate method consistently. It’s designed to keep carbs in the 30-45g range per meal without counting. But if you’re on insulin and need precision, tracking carbs helps. Use apps like the ADA’s "Restaurant Ready" tool to check carb counts for popular chains. It’s 92% accurate and saves time.
What if my friends don’t understand my choices?
It’s common to feel self-conscious. But you don’t need to explain yourself. Just say, "I’m watching my carbs for health reasons," and move on. Most people respect that. If someone pressures you to eat more, it’s okay to say, "I’m full," or "I’m saving room for later." You’re not being rude-you’re taking care of yourself.
Are there any restaurants that are easier for people with diabetes?
Yes. Mediterranean, Japanese, Thai (ask for low-sugar sauces), and grilled seafood places are usually good. Look for menus with lots of vegetables, grilled proteins, and minimal sauces. Chains like Chipotle, Panera Bread, and True Food Kitchen offer carb counts and customizable bowls. Avoid buffets, all-you-can-eat places, and bakeries-those are high-risk zones.
Can I have dessert occasionally?
Absolutely-but plan for it. Skip the bread or rice at dinner so you have room for a small portion. Share a dessert with the table. Choose fruit-based options like berries with whipped cream over cake or ice cream. A small scoop of sorbet (about 1/2 cup) has 15g carbs. A slice of cake? 50g+. Make the trade-off worth it.
How do I know if my carb count is right for me?
Your ideal carb intake depends on your medications, activity level, and blood sugar goals. Most adults with diabetes aim for 45-60g per meal, but some need less-especially if they’re on insulin. Talk to your doctor or a certified diabetes educator. Check your blood sugar two hours after eating. If it’s under 180 mg/dL, you’re on track. If it’s consistently higher, adjust your portions or carb choices.
Eating out with diabetes isn’t about restriction. It’s about awareness. You’re not giving up joy-you’re making smarter choices so you can keep enjoying life. The food doesn’t change. Your approach does. And that’s the difference.

Comments (10)