Complementary Therapy Selector for Hemophilia
Key Takeaways
- Standard clotting factor replacement remains the cornerstone of Hemophilia care.
- Complementary therapies can help with pain, joint health, and stress, but evidence varies.
- Safety is critical - always discuss any new approach with your hemophilia treatment team.
- Acupuncture, tailored physical therapy, and certain nutrition tweaks have the strongest research backing.
- Keep a simple checklist to track benefits, side effects, and communication with clinicians.
Understanding Hemophilia is a genetic bleeding disorder caused by deficiency of clotting factor VIII (Hemophilia A) or IX (Hemophilia B). People with the condition experience prolonged bleeding after injury, surgery, or even routine activities, and they are prone to joint damage from repeated bleeds.
Worldwide, the World Federation of Hemophilia estimates roughly 400,000 individuals live with Hemophilia, with about half in low‑ and middle‑income countries where access to factor concentrates can be limited. Modern care-regular factor infusions, prophylaxis, and comprehensive hemophilia treatment centers-has dramatically improved life expectancy. Yet many patients still battle chronic pain, joint stiffness, and anxiety about bleeding events.
Why Look Beyond Conventional Treatment?
Even with the best available factor therapy, some patients feel gaps in their daily wellbeing. Reasons for exploring alternative medicine a broad umbrella that includes non‑pharmacologic, culturally rooted, and “whole‑person” practices. include:
- Desire for natural or non‑invasive options to manage pain and inflammation.
- Interest in boosting overall immune health and reducing infection risk.
- Stress reduction - mental tension can amplify perceived pain.
- Limited access to factor products in some regions, prompting adjunctive strategies.
It’s crucial to treat complementary approaches as supplements, not replacements, for factor replacement therapy.
Popular Complementary Therapies and What the Evidence Says
Below are the most commonly discussed options among hemophilia patients. Each paragraph introduces the therapy with a short definition, typical use, and a snapshot of scientific support.
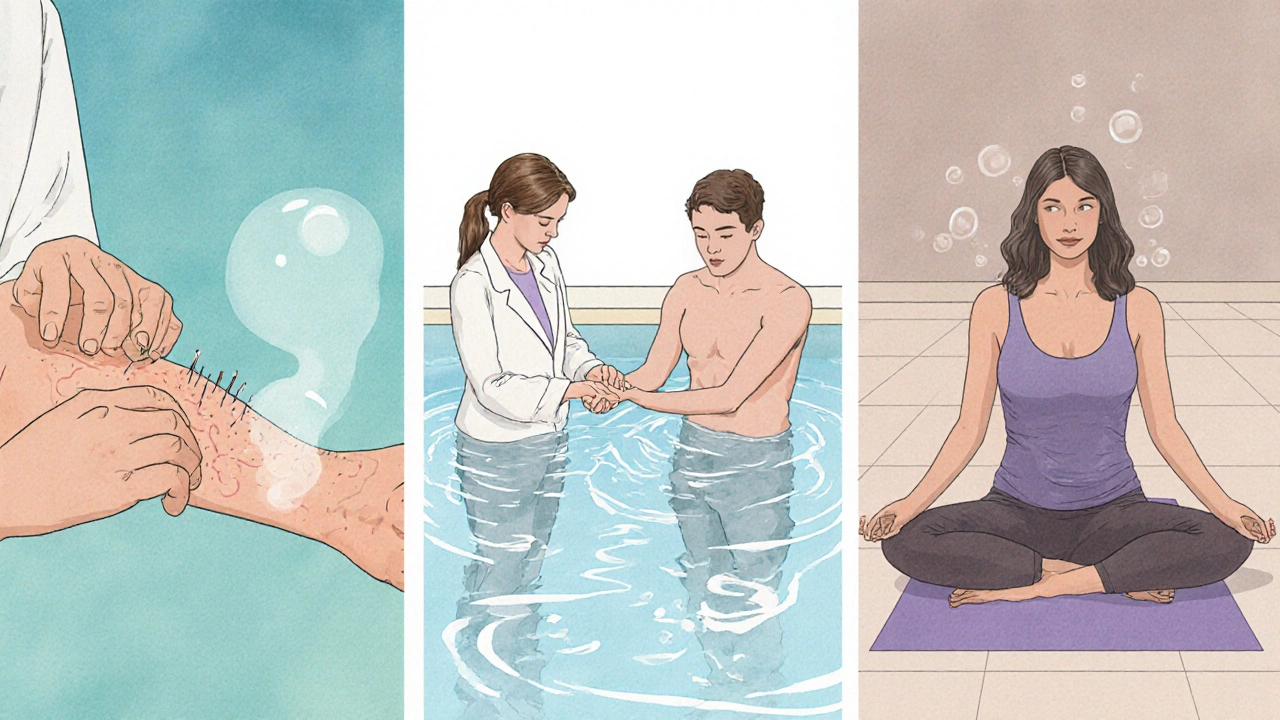
Acupuncture a traditional Chinese technique that inserts thin needles at specific points to modulate pain pathways.
Several small trials in hemophilia cohorts report reduced joint pain scores after a series of weekly sessions, especially for ankles and knees. The mechanism is thought to involve endorphin release and improved micro‑circulation. Safety hinges on using sterile, single‑use needles and avoiding sites with recent bleeds.
Physical Therapy structured exercises and manual techniques aimed at preserving joint range of motion and muscle strength.
Physiotherapy is widely endorsed by hemophilia treatment centers. Evidence shows that individualized programs reduce the frequency of hemarthrosis (joint bleeds) by up to 30% when combined with prophylaxis. Low‑impact activities-swimming, cycling, and guided resistance training-are safest.
Herbal Supplements plant‑derived products such as turmeric, ginger, and devil’s claw advertised for anti‑inflammatory effects.
Laboratory data suggest curcumin (turmeric) can inhibit certain inflammatory pathways, but human trials in hemophilia are scarce. The biggest concerns are potential interactions with anticoagulant medications and unpredictable purity of over‑the‑counter products.
Vitamin K a fat‑soluble vitamin essential for synthesis of clotting factors II, VII, IX, and X.
Patients with mild Hemophilia B sometimes ask whether boosting vitamin K intake can improve clotting. While adequate dietary vitamin K supports baseline factor production, it does not replace missing factor VIII or IX. Large doses have not shown clinical benefit and may interfere with anticoagulant therapy.
Mind‑Body Therapy practices like meditation, yoga, and guided imagery that aim to reduce stress and improve coping.
Randomized studies in chronic pain populations (including a 2022 hemophilia pilot) demonstrate modest improvements in pain perception and quality of life after eight weeks of yoga‑based breathing and gentle stretching. These modalities are low‑risk when movements avoid stressing vulnerable joints.
Homeopathy a system that uses highly diluted substances with the intention of triggering a healing response.
Systematic reviews consistently find no credible evidence that homeopathic remedies affect clotting or bleeding outcomes. While generally safe due to extreme dilution, reliance on homeopathy in place of factor therapy can be dangerous.
Quick Comparison of the Main Options
| Therapy | Potential Benefit | Evidence Strength | Safety Considerations |
|---|---|---|---|
| Acupuncture | Pain reduction, improved joint circulation | Low‑to‑moderate (small RCTs) | Risk of needle‑site bleed; use qualified practitioner |
| Physical Therapy | Enhanced joint stability, fewer bleeds | High (large cohort studies) | Must avoid high‑impact movements during active bleed |
| Herbal Supplements | Anti‑inflammatory, possible pain relief | Very low (mostly animal studies) | Drug‑herb interactions, contamination risk |
| Vitamin K | Supports baseline clotting factor synthesis | Low (nutritional studies only) | Excess can affect anticoagulant dosing |
| Mind‑Body (Yoga, Meditation) | Stress reduction, modest pain improvement | Moderate (pilot RCTs) | Choose low‑impact poses; avoid joint strain |
| Homeopathy | None proven | None (systematic reviews) | Potential delay of effective treatment |
Integrating Complementary Therapies with Standard Care
Here’s a step‑by‑step plan to test a new approach without compromising safety:
- Identify the specific goal (e.g., reduce knee pain).
- Choose one therapy at a time; avoid layering multiple unknowns.
- Consult your hemophilia treatment center. Ask whether the therapy could interfere with factor dosing or bleed risk.
- Start with a short trial-four to six weeks-while keeping a daily log of pain scores, bleed events, and any side effects.
- Review the log with your hematologist. Continue, adjust, or discontinue based on objective outcomes.
Documentation is vital. Many centers now use electronic patient‑reported outcome tools that let you track pain visually and share data instantly with clinicians.

Practical Checklist for Patients and Caregivers
- Medical clearance: Get written approval before starting any new modality.
- Qualified provider: Verify credentials (e.g., licensed acupuncturist with experience in bleeding disorders).
- Bleed safety plan: Have factor concentrate on hand if a needle or stretch triggers a bleed.
- Monitor outcomes: Use a simple chart-pain level 0‑10, any bleeding, medication changes.
- Review schedule: Bring the chart to every clinic visit for objective discussion.
Frequently Asked Questions
Can acupuncture cause a bleed in a hemophilia patient?
Yes, needling a site that has recently bled or is near a joint with known hemarthrosis can trigger bleeding. The key is to work with a practitioner who understands hemophilia, uses sterile single‑use needles, and avoids high‑risk areas.
Are herbal anti‑inflammatories safe alongside factor replacement?
Some herbs (like ginger) can thin blood slightly, potentially increasing bleed risk when combined with certain clotting agents. Always tell your hematologist before adding any supplement, and choose products that have been third‑party tested for purity.
Does yoga help prevent joint bleeds?
Gentle yoga improves flexibility and reduces stress, which can lower perceived pain. It does not prevent bleeds directly, but when combined with prophylactic factor infusions, it contributes to overall joint health.
Should I replace my factor therapy with homeopathic remedies?
No. Homeopathy lacks any credible evidence to affect clotting factor levels. Skipping prescribed factor infusions can lead to life‑threatening bleeds.
What lab tests should I ask for when trying a new supplement?
Baseline CBC (to monitor hemoglobin) and coagulation panels (PT, aPTT) are useful. Repeat the tests after 4‑6 weeks of the supplement to see if any values shift.
Bottom Line
Living with Hemophilia means making educated choices every day. Complementary therapies can fill gaps-especially around pain, joint maintenance, and stress-but they never replace factor replacement. By following a structured trial process, keeping open communication with your care team, and tracking real outcomes, you can safely explore options that fit your lifestyle and improve quality of life.

Comments (13)