Every year, hundreds of thousands of people end up in the hospital not because their illness got worse, but because the medicines meant to help them made things worse. And a big reason? Drug interactions. It’s not just about taking too much of one pill. It’s about what happens when two or more drugs, or even food and supplements, mix inside your body and turn harmless side effects into dangerous ones.
What Happens When Drugs Collide?
Your body doesn’t treat each drug like it’s alone. It tries to process them all at once - breaking them down, moving them around, and getting rid of them. When two drugs interfere with that process, things go sideways. This isn’t rare. About 6% to 30% of all bad reactions to medicines come from these clashes. In 2024, a study of over 500 patients showed that just being on multiple drugs at once raised the chance of a serious side effect by 26%. There are two main ways this happens. The first is called pharmacokinetic - how your body handles the drug. Think of it like traffic on a highway. One drug might block the exit ramp (metabolism), trap another drug in your system, and cause it to build up to toxic levels. The second is pharmacodynamic - how the drug works at its target. Two drugs might both lower blood pressure. Together, they drop it too far. Or one might cancel out the other entirely.The Silent Killer: CYP3A4
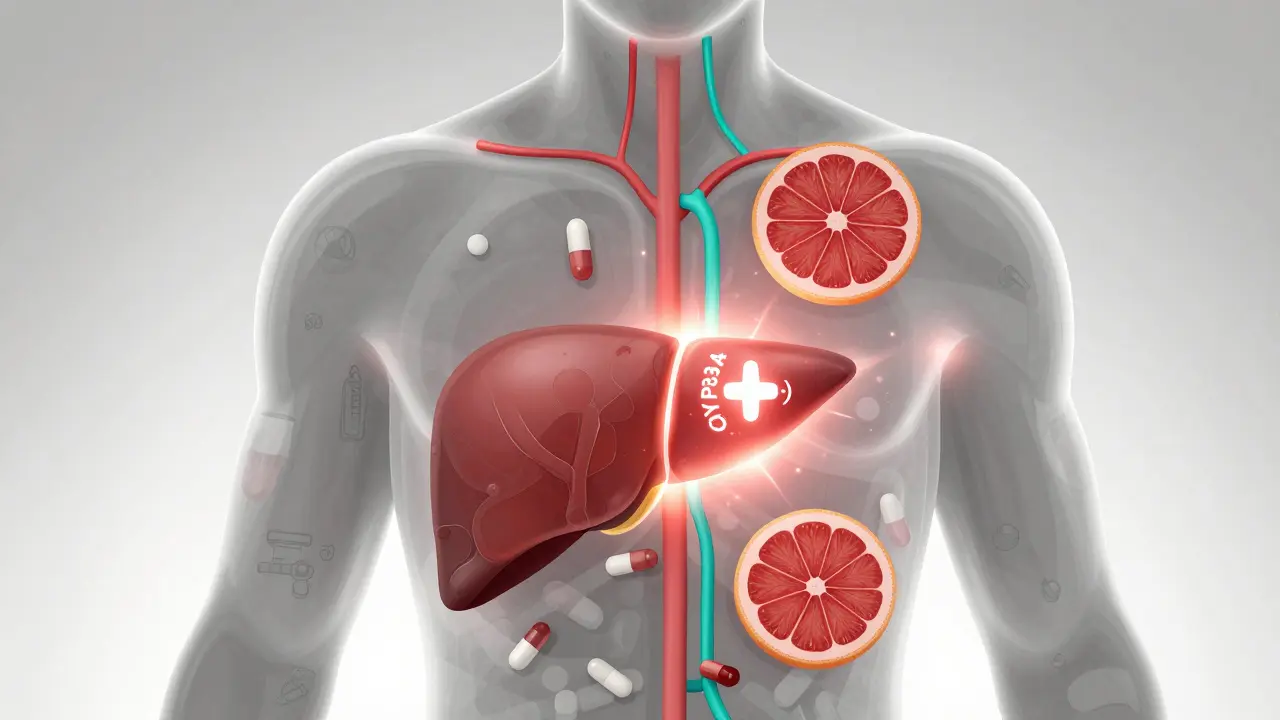
One enzyme system - CYP3A4 - is responsible for breaking down about half of all prescription drugs. That includes statins, blood thinners, antidepressants, and even some cancer meds. When something blocks this enzyme, the drugs don’t get cleared. They pile up. And that’s when trouble starts. Take statins, the cholesterol-lowering drugs. If you’re on simvastatin or atorvastatin and also take clarithromycin (an antibiotic), your risk of muscle damage (rhabdomyolysis) jumps 8.4 times compared to if you took azithromycin, which doesn’t interfere. The numbers are scary: 2.7 out of every 10,000 people on the bad combo get severe muscle breakdown. On the safe one? Only 0.3 out of 10,000. Grapefruit juice is another silent player. It blocks CYP3A4 in your gut. One glass can triple the amount of felodipine (a blood pressure drug) in your blood. That’s not a little bump - it’s enough to send your blood pressure crashing. But not all drugs react the same. Amlodipine? Grapefruit barely touches it. The difference matters.Warfarin: A Balancing Act
Warfarin, a common blood thinner, is one of the most finicky drugs out there. It’s narrow - too little and you clot; too much and you bleed. Many things mess with it. Amiodarone, used for heart rhythm problems, can double your bleeding risk. Even acetaminophen - regular Tylenol - becomes risky if you take more than 2 grams a day. Studies show it bumps up your bleeding risk by almost 80%. And then there’s vitamin K. Found in kale, spinach, broccoli, and supplements, it directly opposes warfarin. If you suddenly start eating more greens or take a vitamin K pill, your INR (a blood test that measures clotting time) drops. Doctors have to adjust your dose constantly. One patient I know went from stable at INR 2.5 to 1.1 in two weeks after starting a green smoothie daily. She almost had a stroke.
Genes Play a Bigger Role Than You Think
Some people are just built differently. About 3% to 10% of white people have a genetic quirk that makes them poor metabolizers of CYP2D6. That’s the enzyme that turns codeine into morphine. If you’re one of them, codeine does nothing. But if you’re a fast metabolizer? You turn it into morphine too fast - and overdose on a regular dose. That’s why some people get dangerously sleepy after taking codeine for a toothache. Others feel nothing. The FDA says 30% of commonly prescribed drugs now come with pharmacogenetic warnings. That means your genes might already be telling your doctor whether a drug is safe for you. But most doctors don’t test for it. Not yet.When Food, Supplements, and Alcohol Jump In
It’s not just other pills. Supplements can be just as dangerous. St. John’s wort, often taken for mild depression, speeds up CYP3A4. That means it can flush out birth control pills, antivirals, and even some cancer drugs before they have time to work. One woman on tamoxifen for breast cancer started taking St. John’s wort for mood swings. Her cancer came back faster. Alcohol? It doesn’t just make you drunk. It can overload your liver. If you’re on acetaminophen, even a few drinks a week can raise your risk of liver failure. If you’re on sedatives or sleeping pills, alcohol multiplies their effect - and that’s how people stop breathing.High-Risk Drug Classes
Some drugs are just more likely to cause trouble. Antiarrhythmics (for irregular heartbeat) have the most interaction potential - over 50 per drug. Blood thinners come next, then antipsychotics and antidepressants. Why? Because they’re narrow-therapeutic-index drugs. That means the difference between a good dose and a toxic one is tiny. A small interaction pushes you over the edge. Cisapride, a drug pulled from the market in 2000, was a nightmare. When taken with antibiotics like erythromycin, it caused fatal heart rhythms in 1.2 out of every 10,000 users. Eighty people died. It wasn’t a fluke. It was predictable. And it happened because no one checked for interactions.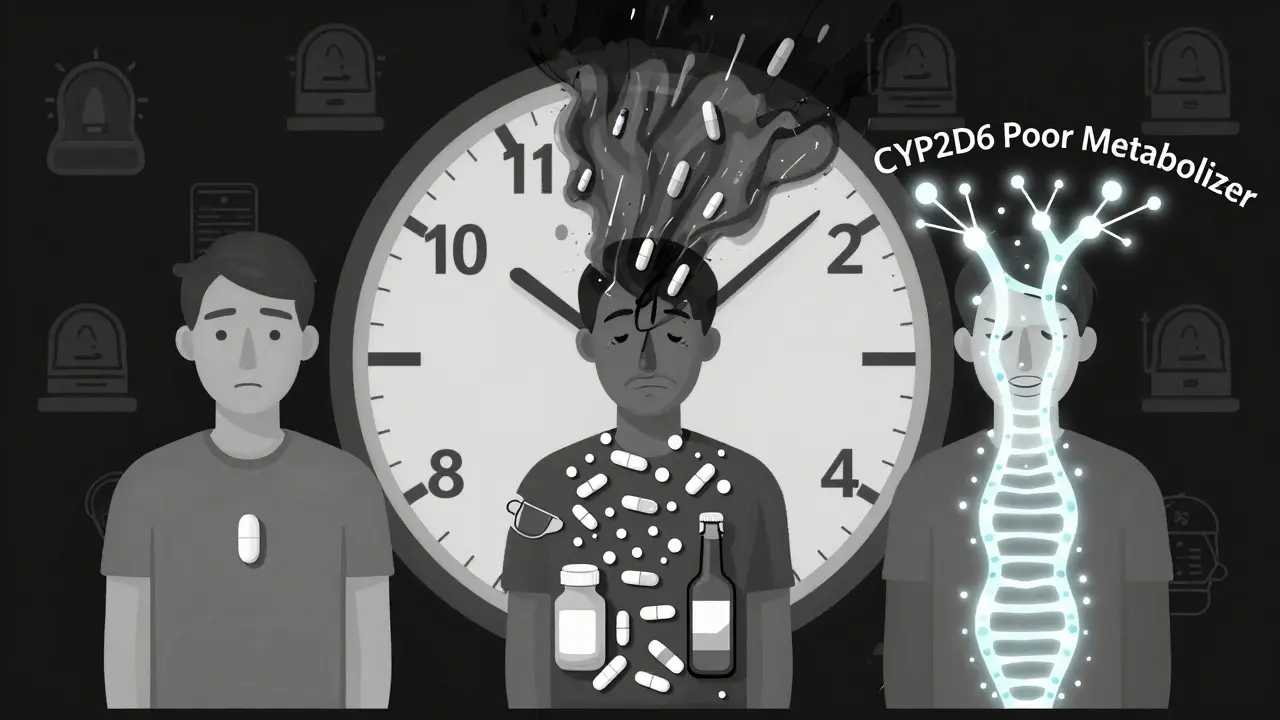
Why Doctors Miss It
You’d think electronic health records would catch all this. They don’t. A 2023 survey of 3,500 doctors found that 74% feel overwhelmed by drug interaction alerts. And here’s the kicker: 90% to 95% of those alerts are ignored. Why? Because most are low-risk noise - like “don’t take ibuprofen with aspirin.” That’s not dangerous for most people. But when every alert sounds the same, doctors tune them out. And when they do miss something? Nurses often catch it first. A 2022 study found that nurses spotted 40% of bad reactions that doctors didn’t. Patients themselves are the last line of defense. If you feel weird after starting a new pill - muscle pain, dizziness, nausea, bruising - don’t assume it’s normal. Ask: “Could this be from something I’m taking with it?”How to Protect Yourself
You don’t need to be a pharmacist to avoid these traps. Here’s what works:- Keep a full list of everything you take. That includes vitamins, herbal supplements, and over-the-counter meds. Even melatonin or magnesium.
- Bring that list to every appointment. Not just your doctor - your dentist, pharmacist, ER doctor.
- Ask your pharmacist. They’re trained to spot interactions. And they’re cheaper than an ER visit.
- Use a single pharmacy. That way, your meds are all in one system. If you use two, the risk of missed interactions doubles.
- Know your high-risk combos. Statin + grapefruit. Warfarin + vitamin K. SSRIs + tramadol (can cause serotonin syndrome). These are red flags.
The Future Is Personal
New tools are coming. AI models now predict dangerous drug combos with 89% accuracy - better than human pharmacists in some cases. Wearable sensors are being tested to track how fast your body clears drugs like warfarin in real time. And pharmacogenetic testing? It’s moving from labs into clinics. Some hospitals now test patients for CYP2D6 and CYP2C19 before prescribing antidepressants or pain meds. But the biggest change? Awareness. The CDC says drug interactions cost the U.S. $9 to $15 billion a year. That’s not just money. It’s hospital beds. It’s lost time. It’s lives. And the scary part? Up to half of these reactions are completely preventable. You don’t need to memorize every drug interaction. But you do need to ask the right questions. And you need to speak up if something feels off. Your body isn’t just reacting to one pill. It’s reacting to the whole mix. And that’s something you can control.Can over-the-counter drugs cause dangerous interactions?
Yes. Common OTC meds like ibuprofen, naproxen, and even antacids can interact. Ibuprofen can increase bleeding risk when taken with warfarin. Antacids with calcium or magnesium can block absorption of antibiotics like tetracycline and fluoroquinolones. Even cold medicines with pseudoephedrine can raise blood pressure dangerously if you’re on certain antidepressants. Always check labels and ask a pharmacist before mixing OTC drugs with prescriptions.
How long do drug interactions last?
It depends on the drug. Some interactions last only as long as both drugs are in your system - a few hours to a couple days. But others can linger. For example, if you take clarithromycin (which blocks CYP3A4), its effect can last up to a week after you stop it. Grapefruit juice can inhibit CYP3A4 for 24-72 hours. Even after you stop eating grapefruit, the enzyme doesn’t recover right away. That’s why timing matters - it’s not just what you take, but when.
Are natural supplements safer than prescription drugs?
No. Many people assume supplements are harmless, but that’s dangerous. St. John’s wort can make birth control, HIV meds, and transplant drugs fail. Kava can cause liver damage when mixed with alcohol or acetaminophen. Garlic and ginkgo can thin your blood and increase bleeding during surgery. Just because something is “natural” doesn’t mean it’s safe - or that it won’t interfere with your meds.
Why do some people have worse side effects than others?
Genetics, age, liver and kidney function, and other health conditions all play a role. Older adults often have slower metabolism and take more meds. People with liver disease can’t break down drugs as well. And as we’ve seen, some people have genetic variants that make them poor or ultra-rapid metabolizers. That’s why two people on the same drugs can have totally different reactions. One gets sick, the other doesn’t - and it’s not random.
Should I stop taking a drug if I suspect an interaction?
Never stop a prescription drug on your own. Some medications, like blood pressure or seizure drugs, can cause serious withdrawal effects. Instead, call your doctor or pharmacist. Describe your symptoms and list everything you’re taking. They can help you decide whether to adjust the dose, switch drugs, or monitor more closely. It’s always safer to get professional advice than to guess.