When a doctor hands you a prescription, what do you really know about what you’re supposed to do? Do you know why you’re taking it? When you’ll feel better? What side effects are normal-and which ones mean you should call? Too often, the answer is no. And that’s not because patients aren’t trying. It’s because the conversation rarely goes deep enough.
Medication misunderstandings are one of the biggest reasons people stop taking their pills. The World Health Organization says about half of people with long-term conditions don’t take their meds as prescribed. That’s not laziness. It’s confusion. And it’s costing the U.S. health system $300 billion a year in avoidable hospital visits, emergency care, and worsening disease.
Start by Asking, Not Telling
Before you explain anything, ask: “What has your doctor told you about this medication so far?” This isn’t just polite-it’s essential. You might think the patient already knows the basics. But in reality, many leave the office with half-remembered fragments, mixed-up instructions, or even wrong ideas. One patient thought their blood pressure pill was for weight loss. Another believed their diabetes medication would cure the disease. Neither was true. And both were at risk.
By asking first, you uncover what they already believe. That lets you correct myths, fill gaps, and build on what they already understand. It also signals: “Your voice matters here.” That’s the foundation of trust.
Use Plain Language-No Jargon Allowed
Forget “take PO BID.” Forget “antihypertensive.” Forget “metabolic pathway.” Those terms don’t help. They confuse.
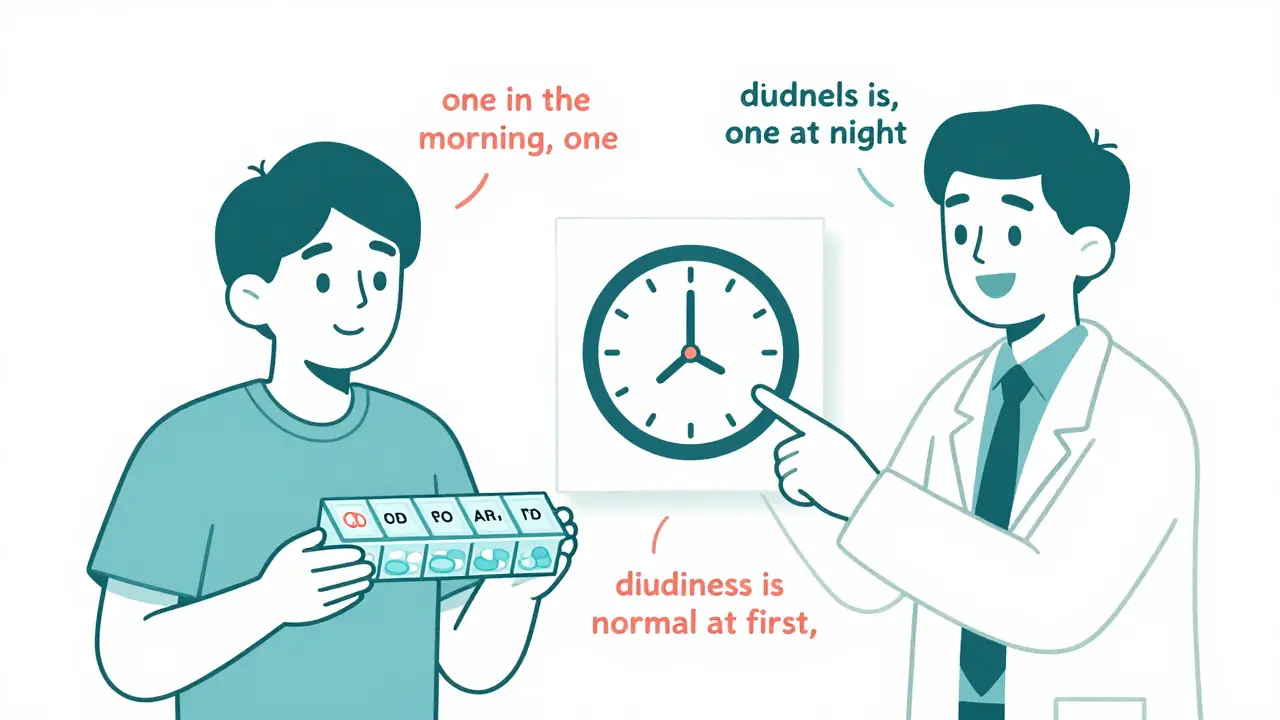
Instead, say: “Take one pill when you wake up and one when you go to bed.” “This medicine helps lower your blood pressure so your heart doesn’t have to work as hard.” “You might feel a little dizzy at first-that’s normal and should go away in a week.”
Research shows that when providers use plain language, patients remember 87% more of what’s said. The American Medical Association found that specific timing instructions-like “with breakfast” or “before bed”-lead to better adherence than vague ones like “take twice daily.”
And here’s something most providers don’t realize: patients don’t need to know how the drug works at a cellular level. They need to know how it affects them. So skip the biochemistry. Say: “This pill helps your body stop holding onto extra salt and water, so your swelling goes down.” That’s what matters.
Quantify Expectations-No Vague Promises
“You’ll feel better soon” is meaningless. How soon? A day? A week? A month?
Be specific. Say: “Most people start noticing less joint pain in 2 to 3 weeks.” “Your cholesterol numbers should drop by about 20% in 6 weeks.” “This insulin helps keep your sugar steady through the day, so you won’t feel shaky after meals.”
And when talking about risks, use absolute numbers-not percentages that sound bigger than they are. Don’t say: “This reduces your risk of heart attack by 30%.” That sounds impressive. But if their baseline risk was 10%, and the medicine lowers it to 7%, that’s a 3 percentage point drop. Say: “Out of 100 people like you, 10 would have a heart attack in 10 years without this medicine. With it, only 7 would.” That’s real. That’s clear.
Use the Teach-Back Method-Don’t Assume Understanding
Teach-Back isn’t a test. It’s a safety net.
After you explain, say: “To make sure I explained this right, could you tell me in your own words how you’ll take this pill?” Or: “What would you tell your spouse about when to take this?”
If they say: “Take it when I feel dizzy,” you’ve caught a dangerous misunderstanding. If they say: “One in the morning, one at night, even if I don’t feel bad,” you know they get it.
The Joint Commission says this simple step increases adherence by 23%. It’s not magic-it’s verification. And it’s now required by Medicare for high-risk medications under the 2025 Merit-Based Incentive Payment System. Providers who skip it risk losing bonuses.
Use Visuals and Hands-On Checks
Words alone aren’t enough. Show them. Use a pill organizer. Point to the actual bottle. Draw a quick clock on paper: “Here’s your morning dose. Here’s your night dose.”
For inhalers, nebulizers, or injectables: have them demonstrate. Don’t just watch-ask: “Show me how you’d use this if you were at home alone.” Most patients think they know how. But in a 2021 UCSF study, nearly half made at least one critical mistake when asked to show their technique.
One nurse in Cape Town started keeping a small whiteboard in exam rooms. She’d sketch the body, mark where the drug works, and draw arrows showing timing. Patients remembered more. And they came back for follow-ups because they felt heard.
Build Time Into Your Schedule
Most primary care visits last 15 to 18 minutes. That’s not enough to cover blood pressure, diabetes, cholesterol, and five new meds. So what do you do?
Don’t try to cram it all in. Schedule dedicated medication review visits. The Royal Australian College of General Practitioners found that clinics doing this saw a 37% improvement in communication quality. Pharmacists can help too-especially for patients on five or more medications. At the Cleveland Clinic, pharmacist-led reviews cut hospital readmissions by 22%.
If you can’t schedule extra time, use the “Chunk and Check” method. Talk for 2-3 minutes. Then stop. Ask: “What stood out to you?” Then move to the next chunk. Johns Hopkins found this boosted patient recall from 36% to 79%.
Listen to the Silence
Patient feedback tells a clear story: 78% of people who felt they understood their meds said their provider used examples they could relate to. And 63% said they didn’t feel like they could ask questions-even if the visit ran just two minutes over.
That silence? It’s not agreement. It’s fear. Fear of sounding stupid. Fear of wasting time. Fear of being judged.
So pause. Wait. Say: “I know this is a lot. What’s the one thing you’re most worried about?” Or: “Is there anything I didn’t explain well?” Let them fill the space. That’s where the real problems surface.

What Happens When You Do This Right?
At Kaiser Permanente, using a simple 5-step protocol-ask, explain, quantify, show, verify-boosted 30-day medication adherence from 62% to 84% in patients with chronic conditions.
At Harvard Medical School, training providers to replace “You must take this” with “Many patients find it helpful to take this with breakfast” reduced readmissions by 29%.
And in clinics that document patient understanding in the medical record, no-show rates dropped by 15%. Why? Because patients who understand their meds feel more connected. They trust their care team. They show up.
This isn’t extra work. It’s better work. It’s the kind of care that saves lives, cuts costs, and makes people feel respected.
What’s Changing Now
Technology is catching up. Electronic health records now have built-in templates to document medication goals. Text reminders are starting to include personalized cues: “Remember we talked about dizziness? That’s normal at first.”
And AI is being tested. At Mayo Clinic, a tool listens to real patient visits and flags when Teach-Back was skipped. In early trials, it caught 92% of missed opportunities.
But the core hasn’t changed. It’s still about talking clearly. Listening deeply. And making sure the patient walks out knowing exactly what to do-and why.
Because when patients understand their meds, they take them. And when they take them, they live better.
Why is it important to avoid medical jargon when explaining medications?
Medical jargon like “BID,” “PO,” or “antihypertensive” is meaningless to most patients. Research shows 80 million American adults have limited health literacy, and even those with higher literacy struggle with unfamiliar terms. Using plain language-like “take one pill in the morning and one at night”-makes instructions clear and actionable. Studies confirm that patients remember 87% more when providers avoid jargon and speak in everyday terms.
What is the Teach-Back method and why is it so effective?
Teach-Back is when you ask the patient to explain back, in their own words, what they need to do with their medication. It’s not a quiz-it’s a way to check understanding. The Joint Commission says it increases medication adherence by 23% because it catches misunderstandings before the patient leaves. If they say, “I take it when I feel sick,” but you meant “take it every day,” you can fix it right then. It’s simple, free, and backed by decades of evidence.
How can I explain medication benefits without making risks sound too scary or too small?
Always use absolute numbers, not relative ones. Instead of saying “This reduces your risk by 50%,” say: “Out of 100 people like you, 10 would have a heart attack in 10 years without this medicine. With it, only 5 would.” That gives real context. Avoid vague phrases like “low risk” or “very safe.” Instead, say: “About 1 in 20 people might feel a little dizzy at first, but it usually goes away after a few days.” Clear numbers build trust.
What should I do if a patient says they don’t want to take their medication?
Don’t argue. Ask why. Often, it’s not about the drug-it’s about side effects, cost, fear, or past bad experiences. Say: “Help me understand what’s making you hesitant.” Then listen. You might find they’re worried about weight gain, drowsiness, or think it’s not working. Once you know the real reason, you can address it: adjust timing, switch to a cheaper option, or explain how the side effect fades. Sometimes, the solution is a different pill. Other times, it’s just reassurance.
How do I fit medication communication into a short appointment?
You don’t need to do it all in one visit. Use the “Chunk and Check” method: cover just two or three key points per visit. For example, focus on purpose and timing today, then side effects and follow-up next time. Schedule separate medication review visits if possible-clinics that do this see 37% better outcomes. Also, use pharmacists for complex regimens. They’re trained to spend 20-30 minutes reviewing meds and can free up your time for other issues.
Can digital tools help with medication communication?
Yes. Automated text reminders that reference your conversation-like “Remember we talked about dizziness? That’s normal at first”-boost adherence. Electronic health records now have templates to document what was discussed. Some systems even flag if Teach-Back wasn’t used. But tools don’t replace conversation-they support it. The most effective systems combine clear talking with smart reminders and easy-to-use visuals.
What’s the biggest mistake providers make when explaining medications?
The biggest mistake is assuming the patient understood. Saying “Does that make sense?” and nodding when they say “yes” isn’t enough. Many patients say yes to avoid embarrassment or because they think they should know. The real solution is Teach-Back: asking them to explain it back. That’s the only way to know for sure. Skipping this step leads to errors, nonadherence, and preventable hospital visits.
Next Steps for Providers
Start small. Pick one patient this week and use Teach-Back. Replace one vague instruction with a specific one. Write down what you discussed about timing and purpose in the chart. That’s it.
Over time, these small changes add up. You’ll see fewer missed doses. Fewer emergency visits. More patients who feel confident, informed, and in control.
Good communication doesn’t require fancy tools or extra staff. It just requires slowing down enough to make sure the person in front of you really understands.
