Neuropathic pain isn't just discomfort-it's your nerves firing off signals like a broken alarm. You might feel burning, stabbing, or electric shocks without any obvious trigger. Even a light touch, like sheets against your skin, can feel unbearable. This isn't normal pain. It's the result of damaged or diseased nerves, often from diabetes, shingles, surgery, or injury. About 1 in 10 people live with it, and for many, traditional painkillers like ibuprofen or even opioids barely help. That's where gabapentin and pregabalin come in. These aren't your typical pain meds. They work on the nerves themselves, quieting the chaos. But which one works better? And which one is right for you?
How Gabapentin and Pregabalin Actually Work
Both gabapentin and pregabalin are cousins in the same drug family. They were originally designed as epilepsy treatments, but doctors noticed they also calmed nerve pain. Their real target? Voltage-gated calcium channels in your spinal cord and brain. These channels are like gates that control how much pain signal gets sent. When nerves are damaged, the gates stick open, flooding your system with pain signals. Gabapentin and pregabalin latch onto the alpha-2-delta subunit of these channels, helping them close. Less calcium gets in, fewer neurotransmitters get released, and the pain signal slows down.
The big difference? Pregabalin binds to these sites six times more tightly than gabapentin. That means it works faster and more predictably. Gabapentin’s absorption is messy-it doesn’t always get absorbed the same way depending on how much you take or whether you ate. Pregabalin? It’s absorbed completely and consistently, no matter what. That’s why doctors often say pregabalin is more reliable.
Effectiveness: Who Gets More Relief?
Studies show both drugs help, but pregabalin has a slight edge. In diabetic nerve pain, about 35% of people taking pregabalin get at least half their pain relief. With gabapentin, it’s closer to 30%. That might not sound like much, but in chronic pain, even 5% more relief can mean the difference between sleeping through the night and lying awake.
A 2021 analysis of over 4,000 patients found that 300 mg of pregabalin gave the same pain relief as 3,600 mg of gabapentin. That’s a huge difference in pill count. Pregabalin also works faster. In one trial, patients reached their effective dose in just over 8 days. With gabapentin, it took nearly 15 days. For someone in constant pain, those extra days matter.
But here’s the catch: effectiveness isn’t just about numbers. A 2024 analysis of patient reports from PatientsLikeMe showed pregabalin scored higher on pain relief (6.2/10) but lower on tolerability (4.8/10). Gabapentin scored slightly lower on relief (5.7/10) but higher on tolerability (5.9/10). One person on Reddit said pregabalin dropped their pain from 8/10 to 3/10 in two days-but they gained 12 pounds in six weeks. Another switched from gabapentin because it made them so dizzy they fell twice. Neither drug is perfect. It’s about trade-offs.
Dosing and Convenience
Gabapentin is a hassle. Because it leaves your body quickly (half-life of 5-7 hours), you have to take it three times a day. That’s hard to remember. Miss a dose? The pain can creep back fast. Many patients stop taking it simply because the schedule is too complicated. The extended-release version, Gralise, helps-it’s once daily-but it’s not available in every pharmacy and costs more.
Pregabalin? Twice daily. Simpler. The newer extended-release version, Lyrica CR, is even better-once daily. That’s a big win for people juggling jobs, kids, or memory issues. Titration is easier too. You start at 75 mg and bump up every few days. With gabapentin, you might start at 100 mg and slowly add 100-300 mg every few days. That’s a lot of adjustments. One 2024 study found primary care doctors took nearly 12 days to get patients on the right dose of gabapentin. With pregabalin, it was under 6 days.

Side Effects: What You’ll Actually Feel
Both drugs cause dizziness, sleepiness, and swelling in the legs. But pregabalin has higher rates of all of them. About 32% of people on pregabalin get dizzy. With gabapentin, it’s 26%. Somnolence? 23% vs. 19%. Peripheral edema? Nearly 11% for pregabalin, less than 10% for gabapentin.
The biggest difference? Weight gain. Pregabalin causes it in over 12% of users. Gabapentin? Just over 3%. That’s not just cosmetic-it can worsen diabetes, increase blood pressure, and make mobility harder. For someone with diabetic neuropathy, gaining 10 pounds can undo progress made with diet and exercise.
There’s also a risk of withdrawal. Stopping either drug suddenly can trigger seizures. That’s why you have to taper off slowly, even if you feel fine. Pregabalin has an added layer of caution: it’s classified as a Schedule V controlled substance in the U.S. because of misuse potential. Gabapentin is not. That means refills are limited, prescriptions are tracked, and some pharmacies may refuse to fill it without extra documentation. For some patients, that’s a barrier to care.
Cost: The Real-World Factor
Gabapentin wins here, hands down. A 90-day supply of 300 mg capsules costs around $16 at most U.S. pharmacies. Generic pregabalin? Around $28 for 60 capsules of 75 mg. That’s nearly double. For people on Medicare or without insurance, that’s a major decision point. A 2024 GoodRx report showed gabapentin is 30-50% cheaper than pregabalin. In safety-net clinics and rural areas, gabapentin is still the default because of cost.
But here’s the twist: cost isn’t just the sticker price. If gabapentin makes you dizzy and you fall, you might end up in the ER. If pregabalin makes you gain weight and your diabetes worsens, you might need more meds or doctor visits. One study found 35% of people on gabapentin stopped taking it because of side effects or complexity. Only 28% stopped pregabalin-but for different reasons: mostly cost and weight gain.
Who Gets Which Drug?
There’s no one-size-fits-all. The American Diabetes Association recommends pregabalin as first-line for diabetic nerve pain because of its consistent dosing and proven results. The Neuropathic Pain Special Interest Group (NeuPSIG) says both are first-line, but recommends choosing based on patient factors.
If you’re young, active, and worried about weight gain, gabapentin might be better-even if it takes longer to work. If you’re older, have trouble remembering to take pills three times a day, or have other conditions that make dosing tricky, pregabalin’s simplicity wins. If cost is tight and you’re on Medicare, gabapentin is often the only practical choice.
Doctors also look at kidney function. Both drugs are cleared by the kidneys. If your eGFR is below 60, doses must be lowered for both. But pregabalin’s dosing adjustments are simpler to calculate.
What’s Next for These Drugs?
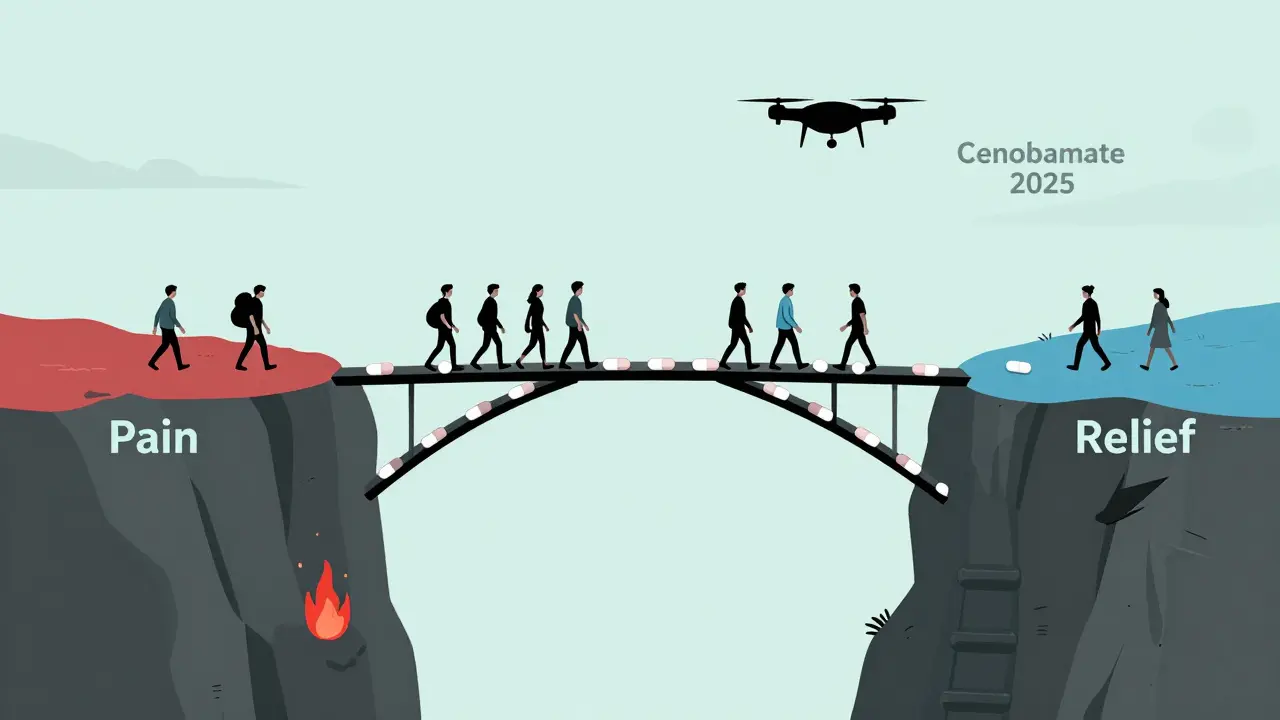
Neither drug is new. Gabapentin’s patent expired decades ago. Pregabalin’s expired in 2019. Generic versions are everywhere. But new options are coming. Drugs like duloxetine (an SNRI) and newer anticonvulsants like cenobamate are showing promise with fewer side effects. The 2025 NeuPSIG guidelines might move gabapentin and pregabalin to second-line for some types of nerve pain. But for now, they’re still the backbone of treatment.
Why? Because they work. They’re safer than opioids. They don’t cause addiction the way opioids do. And for millions of people, they’re the only thing that brings relief. Even with side effects, many would rather have dizziness than burning feet all night.
Real Stories, Real Choices
One woman, 62, with diabetic neuropathy, switched from gabapentin to pregabalin after three months of dizziness and falls. “I went from falling twice a week to walking without fear,” she said. “But I gained 15 pounds. I had to start going to the gym just to stay healthy.”
A 48-year-old man on fixed income switched from pregabalin to gabapentin after his insurance denied coverage. “It took weeks to get used to it,” he said. “But I didn’t gain weight, and I can afford it. I’d rather be slow than broke.”
There’s no perfect drug. Only the right one-for your body, your life, your wallet.
Is gabapentin or pregabalin better for nerve pain?
Pregabalin generally works faster and more reliably, with stronger evidence for pain relief in diabetic and postherpetic neuropathy. Gabapentin is less expensive and causes less weight gain. The best choice depends on your symptoms, cost, ability to follow a dosing schedule, and side effect tolerance.
Can you take gabapentin and pregabalin together?
Doctors rarely recommend taking both at the same time. They work the same way, so combining them increases side effects-dizziness, sleepiness, swelling-without adding much more pain relief. If one doesn’t work, switching is preferred over stacking.
How long does it take for pregabalin to work for nerve pain?
Many people notice some improvement within 3 to 7 days. Full effect usually takes 2 to 4 weeks. Unlike gabapentin, which can take weeks to titrate up, pregabalin reaches its working dose faster, often within 10 days.
Does gabapentin cause weight gain?
It can, but much less often than pregabalin. Studies show about 3% of gabapentin users gain significant weight, compared to over 12% on pregabalin. If weight is a concern, gabapentin is the safer choice.
Why is pregabalin a controlled substance and gabapentin isn’t?
Pregabalin was classified as Schedule V in 2019 because of reports of misuse, especially when taken with opioids or alcohol. While rare, some people use it for its calming or euphoric effects. Gabapentin has similar potential, but it hasn’t been scheduled federally-though some states have started to regulate it.
What happens if I stop taking pregabalin or gabapentin suddenly?
Stopping abruptly can cause seizures, anxiety, insomnia, nausea, and sweating. Even if you feel fine, you must taper off slowly over weeks under medical supervision. This is true for both drugs. Never stop on your own.
Next Steps: What to Do If You’re on One of These Drugs
If you’re taking gabapentin or pregabalin, keep a symptom journal. Note your pain level daily, any side effects, and whether you missed doses. Bring it to your next appointment. If you’re not getting relief after 4-6 weeks, talk to your doctor about adjusting the dose or trying something else. If you’re gaining weight or feeling too drowsy, don’t just quit-ask for alternatives. There are other options: duloxetine, venlafaxine, topical lidocaine, or even physical therapy. These drugs aren’t magic, but they’re tools. Use them wisely.

Comments (11)