What Is Nociceptive Pain, Really?
Nociceptive pain isn’t just "hurting"-it’s your body’s alarm system kicking in because something’s physically damaged. Think stubbing your toe, pulling a muscle, or having arthritis flare up. This pain comes from real, measurable harm to skin, muscles, tendons, bones, or organs. It’s not caused by nerve damage like neuropathic pain, and it’s not mysterious like nociplastic pain. It’s straightforward: tissue gets injured, chemicals are released, and nerves scream for help.
The International Association for the Study of Pain defines it clearly: pain from actual or threatened damage to non-neural tissue. That means if you cut yourself, sprain your ankle, or get a stomach ulcer, your body’s nociceptors-special nerve endings-detect the damage and send signals to your brain. This isn’t a glitch. It’s survival. Without nociceptive pain, you wouldn’t pull your hand off a hot stove. About 85% of all acute pain cases fall into this category, according to a 2022 meta-analysis in Pain Medicine.
Three Types of Nociceptive Pain (And How They Feel)
Not all tissue injuries are the same, and neither are the pains they cause. There are three main types:
- Superficial somatic pain: Comes from skin or mucous membranes. Sharp, pinpoint, and easy to locate. Think a paper cut or sunburn. It’s carried by fast Aδ fibers that fire off signals at 5-30 meters per second.
- Deep somatic pain: Originates in muscles, joints, tendons, or bones. It’s dull, aching, and harder to pinpoint. A pulled hamstring or fractured rib feels this way. Signals travel slowly via C fibers at just 0.5-2 m/s.
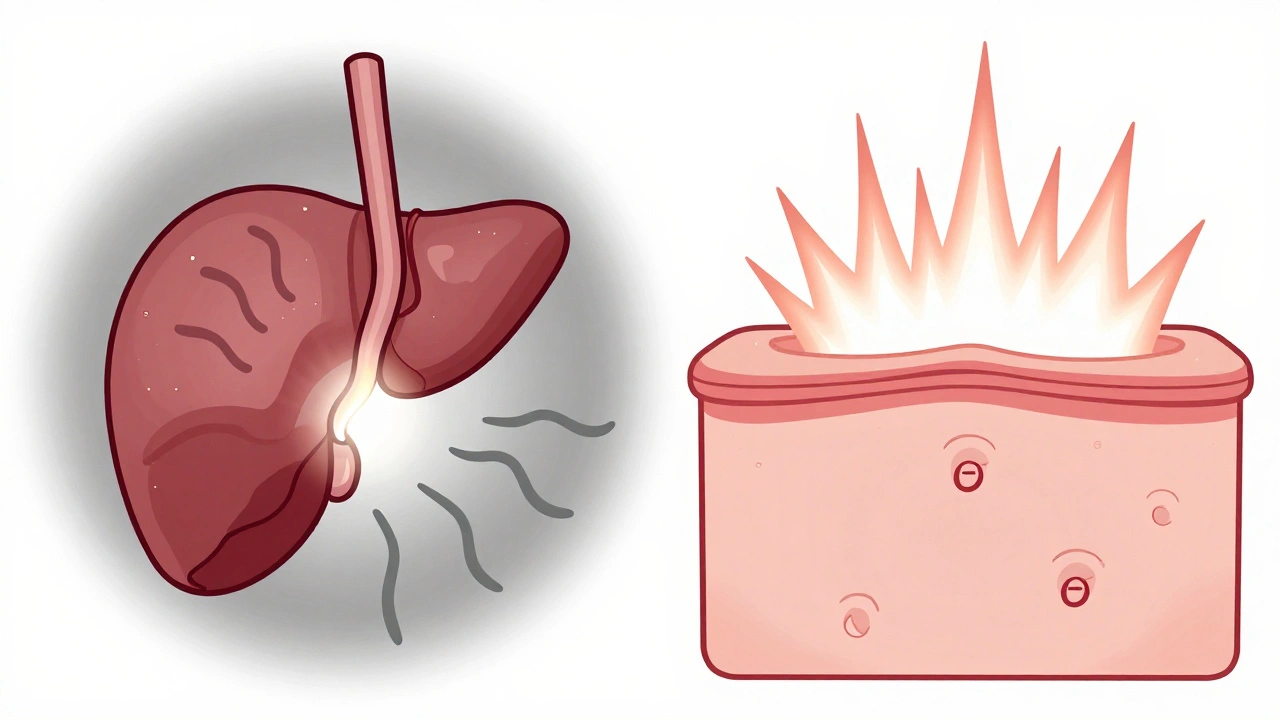
- Visceral pain: Comes from internal organs like the gallbladder, kidneys, or intestines. It’s often described as cramping, pressure, or a deep throb. It’s tricky because organs don’t have many pain receptors-until they get inflamed. Then, dormant nociceptors wake up and start sending signals.
What triggers these? Three things: heat (like burns), pressure (like a crushed finger), and chemicals (like acid from inflammation). In bone cancer, for example, the tissue becomes acidic (pH drops to 6.8-7.0), and that’s enough to activate nociceptors that were previously silent.
NSAIDs: The Inflammation Killers
NSAIDs-like ibuprofen, naproxen, and aspirin-work where the pain starts: at the injury site. They block enzymes called COX-1 and COX-2. COX-2 makes prostaglandins, the chemicals that cause swelling, heat, and pain. By stopping them, NSAIDs reduce both inflammation and pain.
A 2023 Cochrane Review looked at 35 studies with over 7,800 people. The result? Ibuprofen 400mg gave 50% pain relief to 49% of patients with acute sprains or strains. Placebo? Only 32%. That’s a clear edge. NSAIDs are especially powerful when there’s visible swelling, redness, or warmth-signs of inflammation.
Doctors at the American College of Rheumatology recommend NSAIDs as first-line treatment for osteoarthritis. Athletic trainers use them routinely after injuries. A 2023 survey found 89% of athletic trainers reach for NSAIDs first for sprains and strains. Why? Because they don’t just mask pain-they help the healing process by reducing swelling, which can speed recovery by 2-3 days, as one physical therapist noted on Reddit.
Acetaminophen: The Quiet Central Player
Acetaminophen (also called paracetamol) doesn’t touch inflammation. It doesn’t reduce swelling. It doesn’t cool down a hot knee. Instead, it works mostly in the brain and spinal cord. It’s thought to block a variant of COX called COX-3 and may also affect serotonin pathways. Some newer research suggests it modulates TRPV1 channels-those same ones that react to heat and capsaicin.
Its strength? It’s gentle on the stomach. No GI irritation. No bleeding risk. That’s why pediatricians and geriatricians prefer it. The American Academy of Pediatrics recommends it as the go-to for kids. Geriatricians use it in older adults because NSAIDs can cause dangerous bleeding or kidney issues in this group.
But here’s the catch: it’s weak against inflammation-driven pain. A 2022 JAMA meta-analysis found acetaminophen helped only 39% of people with acute low back pain. Ibuprofen? 48%. For tension headaches, it’s fine-no inflammation there. But for a swollen ankle? Not enough.
When to Use Which: A Practical Guide
Here’s how to pick:
- Use NSAIDs if: There’s swelling, redness, heat, or stiffness. Sprains, strains, arthritis flares, tendonitis, post-surgical inflammation. Dose: ibuprofen 400-600mg every 6-8 hours for 3-7 days. Start within 2 hours of injury for best results.
- Use acetaminophen if: The pain is dull, constant, and there’s no swelling. Mild headaches, minor muscle soreness, post-viral aches. Dose: 650-1,000mg every 6 hours. Never exceed 3,000mg/day if you have liver issues.
What about combination therapy? A 2022 Mayo Clinic survey found 61% of chronic pain patients took both together-and reported 32% better pain control than either drug alone. That’s smart for mixed pain, like osteoarthritis with flare-ups and general aching.
The Downsides: Risks You Can’t Ignore
NSAIDs aren’t harmless. Long-term use raises your risk of stomach ulcers by 1-2% per year. High doses of diclofenac double your heart attack risk, according to The Lancet. Even over-the-counter ibuprofen can cause kidney damage if taken daily for months. Tinnitus (ringing in the ears) is another underreported side effect.
Acetaminophen’s danger is liver failure. It’s the #1 cause of acute liver failure in the U.S. The safe max is 4,000mg/day-but that’s for healthy adults. If you drink alcohol, have liver disease, or take other meds, cut it to 3,000mg or less. Just 150-200mg/kg can be fatal. That’s 10-14 standard 500mg tablets for a 70kg adult.
Many people don’t realize how easy it is to overdose. Cold medicines, sleep aids, and prescription painkillers often contain acetaminophen. Taking two products with it? You’re at risk.
What’s New in Pain Relief?
Science is catching up. Topical NSAIDs-like diclofenac gel-are gaining traction. They deliver pain relief with only 30% of the systemic exposure of pills, meaning fewer side effects. A 2023 study in Annals of Internal Medicine confirmed they work just as well as oral versions for knee osteoarthritis-with way less stomach trouble.
Then there’s Vimovo: a combo pill with naproxen and a stomach-protecting drug (esomeprazole). The TARGET trial showed it cut ulcer risk by 56%. For people who need long-term NSAIDs, this is a game-changer.
On the acetaminophen front, the FDA approved Qdolo in 2022-a combo of tramadol and acetaminophen-for moderate-to-severe pain. It’s not for everyone, but it gives a middle ground between pure acetaminophen and opioids.
Future drugs? Eli Lilly’s LOXO-435 is in Phase II trials. It targets TRPV1 channels in visceral pain nerves. Early results show 40% pain reduction in irritable bowel syndrome. That’s huge for people who suffer from chronic organ pain with no good options today.
Real People, Real Choices
Reddit’s r/PainMedicine community analyzed 312 posts in 2023. 68% said NSAIDs worked better for acute injuries. One user, u/PhysicalTherapistAmy, wrote: "I tell my patients to take 600mg ibuprofen three times a day for a sprained ankle. The swelling goes down, and they move better by day three."
On Drugs.com, 74% of users rated acetaminophen highly for headaches-mostly because "no stomach upset." But 35% of negative reviews said it "didn’t touch my pain." For moderate pain, it just doesn’t cut it.
Final Take: Know Your Pain, Know Your Medicine
Nociceptive pain isn’t one thing. It’s a signal. And how you treat it should match the signal.
If your knee is swollen and hot after a fall? NSAID. If you’ve got a tension headache and your stomach’s sensitive? Acetaminophen. If you’re dealing with both? A combo can work wonders.
Don’t reach for the bottle blindly. Ask yourself: Is there inflammation? Is the pain sharp or dull? Is my liver okay? Am I taking other meds with acetaminophen? These questions matter more than brand names or price tags.
And remember: pain relief isn’t about feeling better tonight. It’s about healing right, avoiding complications, and not trading one problem for another.

Comments (13)