When you hurt - whether from a bad back, a broken bone, or arthritis that won’t quit - the first question isn’t just what works? It’s what won’t kill me?
Why Opioids Are No Longer the First Choice
For decades, opioids like oxycodone, hydrocodone, and morphine were the go-to for serious pain. But that’s changed. Today, doctors don’t start with opioids unless they absolutely have to. Why? Because the risks don’t match the rewards. A major 2018 study called the SPACE trial followed 240 people with chronic back or joint pain for a full year. Half got opioids. The other half got non-opioid meds like ibuprofen and acetaminophen. At the end? Both groups had nearly the same pain relief. But the opioid group had way more side effects: dizziness, constipation, nausea, and worse - a higher chance of dependence. Even more telling? The non-opioid group actually had slightly better pain scores. And when you look at long-term outcomes, opioids don’t just fall behind - they become dangerous. A study of nearly 300,000 patients found that taking opioids for more than 180 days over three years doubled the risk of a heart attack. Daily doses above 120 mg of morphine equivalent? That risk jumps 58%. That’s not a small side effect. That’s a life-threatening one.Non-Opioids Work Better - And Safer
Non-opioid painkillers aren’t just safer. In many cases, they’re more effective. NSAIDs like ibuprofen and naproxen reduce inflammation. Acetaminophen (Tylenol) blocks pain signals in the brain. Neither causes addiction. Neither slows your breathing. Neither turns your gut into a mess. And now there’s something new: Journavx. Approved by the FDA in March 2024, it’s the first new non-opioid painkiller class in decades. It doesn’t touch opioid receptors. It doesn’t carry addiction risk. In clinical trials, it worked better than placebo for surgical pain - and patients could still take ibuprofen if they needed extra relief. Pediatric research backs this up too. A 2024 review of five studies on kids with broken bones or post-surgery pain found no evidence that morphine or codeine worked better than ibuprofen. But the opioid kids? They had way more vomiting, drowsiness, and even low oxygen levels. For children, non-opioids aren’t just safer - they’re clearly better.The Opioid Epidemic Isn’t Over - It’s Still Killing People
In 2021, over 80,000 Americans died from opioid overdoses. That’s not a statistic. That’s 80,000 families shattered. The CDC declared this a public health emergency in 2017 - and it’s still happening. It’s not just about street drugs like heroin. A huge portion of these deaths started with a prescription. Someone gets a pill for a back injury. Takes it a little longer than needed. Gets used to the feeling. Then the dose creeps up. And one day, the body can’t handle it. Even in places like South Africa, where opioid access is more controlled, the global trend affects local prescribing habits. Doctors here are learning from the U.S. mistake. The message is clear: if you can avoid opioids, do it.What the Guidelines Say Now
Major medical groups have all changed their stance: - The 2022 CDC Clinical Practice Guideline says: Use non-opioid therapy as the preferred treatment for chronic pain. Opioids? Only if everything else fails - and even then, use the lowest dose for the shortest time. - The American College of Physicians admits: There’s little proof opioids help long-term. The risks? Proven. - The VA Health System - which treats hundreds of thousands of veterans - states outright: Opioids aren’t more effective than non-opioids, but they cause far more harm. - California’s Medical Board says: Try physical therapy, NSAIDs, or acetaminophen before even considering opioids. These aren’t opinions. They’re based on hard data from real patients over real time.When Are Opioids Still Appropriate?
This isn’t a blanket ban. There are times opioids make sense. - After major surgery, like a hip replacement or cancer resection - short-term use (a few days) is still common and appropriate. - For cancer-related pain, where the goal is comfort, not long-term function - opioids remain a vital tool. - In palliative care, where quality of life is the only metric that matters. But for lower back pain? Arthritis? Headaches? Sprains? Migraines? There’s almost never a good reason to start with opioids.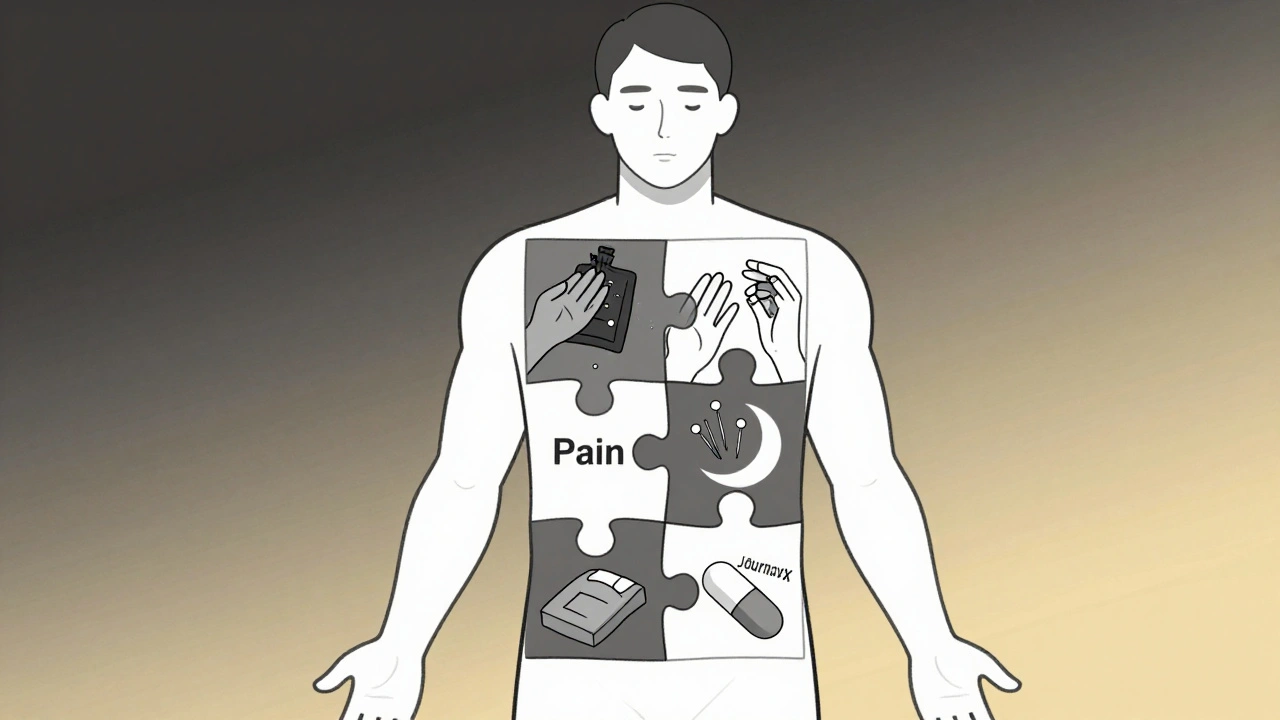
What You Can Do Right Now
If you’re on opioids for chronic pain and wondering if you should switch:- Ask your doctor about NSAIDs or acetaminophen - and whether they’re right for your condition.
- Request physical therapy or movement-based treatments. Movement reduces inflammation and builds natural pain resistance.
- Ask about nerve blocks, acupuncture, or cognitive behavioral therapy. These aren’t "alternative" - they’re evidence-backed.
- If you’ve been on opioids for more than 3 months, get a heart health check. Long-term use increases cardiovascular risk.
- Never stop opioids cold turkey. Talk to your doctor about a taper plan.
What’s Next for Pain Relief?
The future isn’t about stronger opioids. It’s about smarter, safer combinations. Doctors are moving toward multimodal pain management - using several low-risk tools together. Think: NSAID + physical therapy + heat therapy + sleep improvement. That’s more effective than any single pill. The FDA is funding new non-opioid drugs. Researchers are testing topical gels, targeted nerve blockers, and even digital therapies that retrain how the brain processes pain. We’re not going back to the days of "just take a pill." We’re moving toward a system where pain is treated like a system - not just a symptom.Final Thought: Pain Isn’t the Enemy - Risk Is
Pain is your body’s alarm. It’s telling you something’s wrong. But the medicine you take to silence that alarm shouldn’t put you in more danger than the problem itself. Non-opioid options work. They’re safer. They’re cheaper. And now, they’re backed by the strongest guidelines in medical history. You don’t need to suffer. But you also don’t need to risk your life for temporary relief. Ask the right questions. Demand safer options. Your future self will thank you.Are opioids ever safe for long-term pain?
For most people with chronic non-cancer pain - like back pain, arthritis, or headaches - opioids are not safe for long-term use. Studies show they don’t provide better pain relief over time, but they do increase risks of addiction, heart problems, overdose, and death. The CDC and other major health groups now recommend non-opioid treatments as the first and preferred option. Opioids may be appropriate for short-term use after surgery or for cancer-related pain, but even then, they should be used at the lowest dose and shortest duration possible.
Can I just take more ibuprofen instead of opioids?
It’s not about taking more - it’s about taking smart. Ibuprofen and other NSAIDs are effective for many types of pain, especially those involving inflammation like joint pain or muscle strains. But they aren’t risk-free either. Long-term or high-dose use can cause stomach ulcers, kidney damage, or increased blood pressure. The key is using the lowest effective dose for the shortest time. Talk to your doctor about your specific condition. For some people, alternating NSAIDs with acetaminophen or adding physical therapy is safer than relying on one drug alone.
Is Journavx available everywhere?
Journavx was approved by the FDA in March 2024 for acute pain, such as after surgery. It’s not yet widely available in all countries, and its access in places like South Africa depends on local regulatory approval and pharmacy stocking. It’s not meant for chronic pain or everyday use. It’s a targeted option for short-term, moderate-to-severe pain where opioids were traditionally used. Ask your doctor if it’s an option for your situation - but don’t assume it’s a magic bullet. It’s one tool among many.
What are the signs I’m becoming dependent on opioids?
Dependence doesn’t always mean addiction. Signs include needing higher doses to get the same effect, feeling withdrawal symptoms (anxiety, sweating, nausea, insomnia) when you miss a dose, or continuing use even when it’s not helping your pain. If you find yourself taking opioids "just to feel normal" or hiding your use from others, that’s a red flag. Talk to your doctor immediately. Stopping abruptly can be dangerous - but tapering off safely is possible with support.
Can I use non-opioid meds if I have kidney or liver problems?
Yes - but carefully. Acetaminophen can harm the liver if taken in high doses or with alcohol. NSAIDs can strain the kidneys, especially in people with existing kidney disease or high blood pressure. That’s why personalized care matters. Your doctor can adjust doses, recommend alternatives like topical creams, or suggest non-drug options like heat therapy or nerve stimulation. Never assume a "safe" drug is safe for you - always check with your provider based on your health history.
Why do doctors still prescribe opioids if they’re so risky?
Some doctors still prescribe opioids because they were trained to do so, or because patients expect them. Others may lack time or resources to explore alternatives like physical therapy or behavioral pain programs. There’s also lingering pressure from patients who believe stronger drugs mean better care. But the tide is turning. More clinics now offer multidisciplinary pain programs, and guidelines have shifted dramatically since 2016. If your doctor suggests opioids for chronic pain without first discussing safer options, ask why - and consider getting a second opinion.

Comments (13)