Why Infections Are the Biggest Threat After a Kidney Transplant
After a kidney transplant, your new organ works hard to keep you alive-but your immune system is fighting a losing battle. To stop your body from rejecting the new kidney, doctors give you powerful drugs that weaken your defenses. That’s good for the transplant, but terrible for stopping germs. Infections are the leading cause of illness and death in the first year after transplant. You’re not just at risk for a cold or flu-you could get pneumonia, a deadly fungal infection, or a virus like CMV that can destroy your graft. The good news? You don’t have to wait for infection to strike. Prevention starts before surgery and lasts your whole life.
Prevention Starts Before the Transplant
Many people think infection prevention begins after surgery. It doesn’t. It starts months before, during your transplant evaluation. Your medical team checks your vaccination history, screens for hidden infections like hepatitis B or tuberculosis, and tests whether you’ve been exposed to CMV (cytomegalovirus). If you’ve never had CMV but your donor has, you’re in the highest risk group. That’s called D+/R--donor positive, recipient negative. It’s rare, but dangerous. For these patients, doctors start antiviral medicine like valganciclovir before you even leave the hospital. This isn’t optional-it’s standard care.
Before transplant, you’ll also get shots for things you may have missed: pneumococcal vaccine, hepatitis B, and tetanus. If you’re due for the flu shot, you’ll get it early. Live vaccines like MMR or chickenpox? Those are off-limits after transplant. That’s why getting them before surgery is critical. And don’t forget your family. If your spouse or kids aren’t up to date on their flu shots, they could bring home a virus you can’t fight. That’s why doctors recommend a "cocoon"-everyone around you gets vaccinated to protect you.
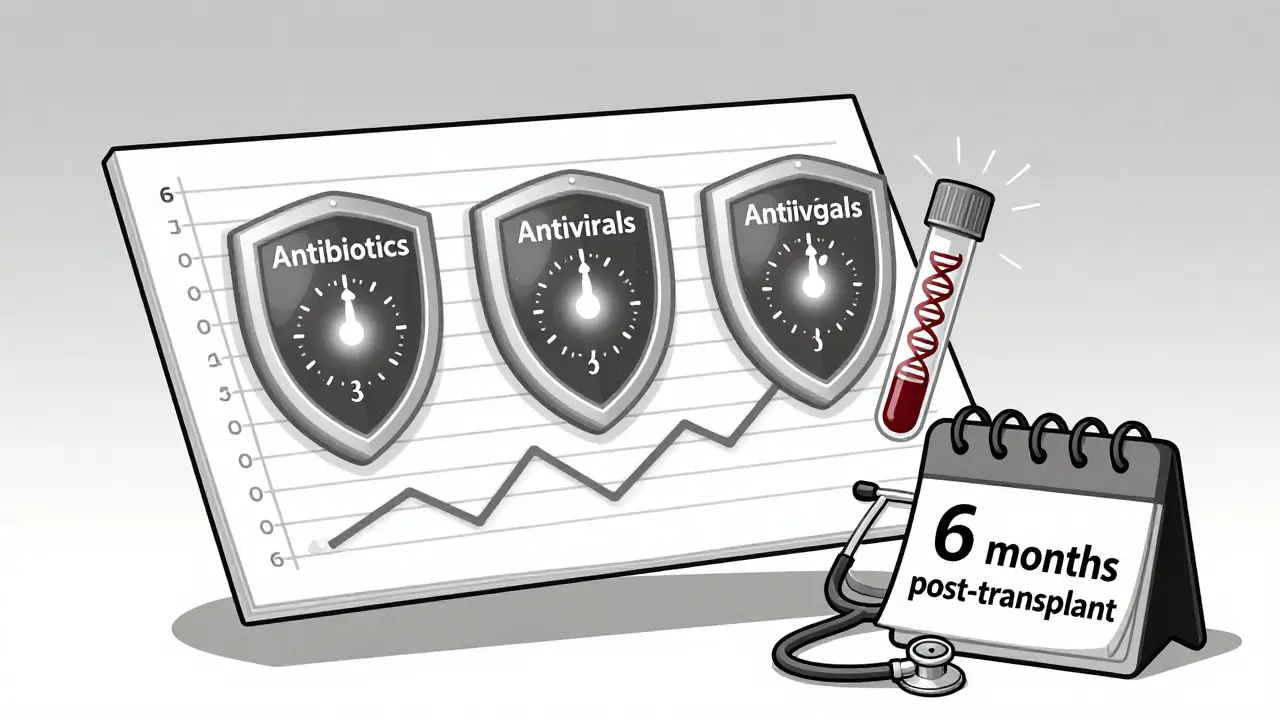
Medicines That Stop Infections Before They Start
After transplant, you’ll be on a schedule of preventive medicines. It’s not random. Each drug targets a specific threat at a specific time.
- Antibiotics: For the first 3 to 6 months, you’ll take trimethoprim-sulfamethoxazole to prevent Pneumocystis jirovecii pneumonia, a deadly lung infection that used to kill half of transplant patients before this drug became routine.
- Antivirals: For CMV, you’ll take valganciclovir for 3 to 6 months. Some high-risk patients stay on it longer. If you’re on preemptive therapy, your blood gets tested every week for CMV DNA. As soon as the virus shows up-even if you feel fine-you start treatment. This cuts infection rates by over 70%.
- Antifungals: If you had a bone marrow transplant or are on heavy immunosuppression, you might get fluconazole to prevent fungal infections like candidiasis. For those in mold-prone areas, like the Ohio River Valley, doctors may add it even after kidney transplant.
These aren’t lifelong drugs. They’re time-limited shields. Once your immune system starts to recover, you stop them. But stopping too soon? That’s when infections creep back in.
What You Must Do Every Day to Stay Safe
Medicines help, but your daily choices matter more. You can’t control your donor’s CMV status. But you can control your kitchen, your hands, and your social circle.
- Food safety: No raw fish, no soft cheeses like brie or camembert, no unpasteurized milk. Listeria doesn’t care if you’re a transplant patient-it only cares if your food is undercooked. Cook meat until it’s steaming hot. Wash fruits and vegetables even if you peel them. Store leftovers within two hours.
- Handwashing: Soap and water for 20 seconds, every time you use the bathroom, before eating, after touching pets. Alcohol gel works when soap isn’t available, but soap is better. You’ll wash your hands more than you brush your teeth.
- Mask up: During flu season, wear a mask in crowded places like supermarkets or hospitals. Respiratory viruses are the #1 infection after transplant. Even a mild cold can lead to pneumonia in your weakened state.
- Pets: Cats and dogs can be part of your life-but no litter boxes. No bird cages. No reptiles. No petting stray animals. If you have a cat, have someone else clean the litter box. Wash your hands after touching your dog. Pets bring joy, but also germs. Balance matters.
And don’t forget your environment. If you garden, wear gloves and a mask. Soil carries fungi like histoplasmosis. If you’re remodeling, stay out of the house until it’s done. Dust is dangerous.
Monitoring: Blood Tests Are Your Early Warning System
You won’t always feel sick before an infection takes hold. That’s why monitoring isn’t optional-it’s your lifeline.
For CMV, weekly blood tests for viral DNA are routine for the first few months. If the number rises, you get antivirals before you have symptoms. For fungal infections, doctors check your blood for galactomannan or beta-D-glucan-proteins that signal fungi are growing. If those markers spike, you get scanned for lung or liver damage before you even cough.
For bacterial infections, especially those from catheters, your team checks your central line site daily. A red spot? A fever? That’s not just a rash-it could be a bloodstream infection. Chlorhexidine-impregnated dressings cut infection risk by up to 22%. But if you don’t change the dressing on time or touch the hub with dirty hands, you undo all that protection.
And don’t ignore routine cultures. If you’re in a hospital with high rates of drug-resistant bacteria, you might get swabs every week. These aren’t scary tests-they’re your early warning system.
Vaccines After Transplant: What’s Safe, What’s Not
After transplant, your immune system is like a car with no brakes. Live vaccines are too risky-they could make you sick. So you wait. Most inactivated vaccines are safe starting at 6 months post-transplant. That includes:
- Influenza (flu shot)
- Tetanus, diphtheria, pertussis (Tdap)
- Pneumococcal (PCV20 or PPSV23)
- Hepatitis A and B
- COVID-19 (mRNA vaccines)
Live vaccines like shingles (Zostavax) are off-limits. But there’s good news: the new shingles shot, Shingrix, is inactivated and safe after 6 months. Get it. Shingles can be brutal for transplant patients.
And don’t assume one shot is enough. You may need boosters. Your doctor will track your antibody levels and adjust your schedule. It’s not one-size-fits-all. Some people need three flu shots in their first year. Others need a second pneumococcal shot a year later.
The New Frontiers: Fighting Superbugs and Rewriting the Microbiome
More than one in three bacterial infections after transplant now come from drug-resistant germs. These aren’t your grandpa’s infections. They’re superbugs-bacteria that laugh at antibiotics. The most common? ESBL-producing E. coli. They hide in your gut and wait for your immune system to drop.
Doctors are fighting back with new tools. Fecal microbiota transplantation (FMT)-yes, poop transplants-is being tested to replace bad gut bacteria with healthy ones. Early results show it can reduce colonization by superbugs by up to 80%. It’s not standard yet, but it’s coming.
Other ideas? Anti-adhesion drugs that stop bacteria from sticking to your bladder. Intravesical therapy that floods your bladder with harmless bacteria to crowd out the bad ones. These aren’t sci-fi-they’re in clinical trials right now.
And the big hope? A CMV vaccine. No one has one yet, but at least five are in human trials. If one works, it could replace lifelong antivirals for thousands of patients.
What Happens After 6 Months? The Long Game
After six months, your immunosuppression gets lighter. Your doses go down. You feel better. That’s when people get careless. "I’m fine," they say. "I don’t need to worry anymore." That’s a trap.
Most infections after transplant happen after the first year. Why? Because the drugs stop. The CMV prophylaxis ends. The antibiotic shield is gone. You go back to work. You hug your grandkids. You eat sushi. And then-bam-you get sick.
That’s why lifelong vigilance matters. You’ll still need:
- Annual flu shots
- Regular blood tests for CMV (at least once a year)
- Good hygiene
- Food safety
- Masking in outbreaks
Your transplant isn’t just a surgery. It’s a lifelong partnership with your care team. The better you understand the risks, the longer your kidney lasts.
What to Do If You Feel Off
Don’t wait. Don’t think it’s just a cold. If you have:
- Fever over 100.4°F (38°C)
- Unexplained fatigue
- Diarrhea lasting more than 2 days
- Cough or shortness of breath
- Red, swollen, or draining area around your incision
Call your transplant center immediately. Don’t wait for your next appointment. Don’t go to the ER unless you’re in crisis. Go to your transplant team. They know your history. They know your risks. And they can act fast.
Can I get the flu shot after a kidney transplant?
Yes, but only the inactivated flu shot, not the nasal spray. You can get it safely starting 6 months after transplant. Get it every year. The flu can turn deadly for transplant patients, and the shot reduces your risk of hospitalization by over 60%.
Is it safe to have pets after a kidney transplant?
Yes, but with limits. Dogs and cats are okay if you avoid litter boxes, don’t let them lick your face, and wash your hands after touching them. Avoid reptiles, birds, and rodents-they carry germs like salmonella and cryptosporidium that can be deadly. If you have a cat, have someone else clean the litter box.
Why do I need to take antiviral drugs after transplant if I feel fine?
CMV often has no symptoms at first-but it can still damage your new kidney. By the time you feel sick, the virus may have already caused inflammation, rejection, or scarring. Taking antivirals like valganciclovir prevents the virus from multiplying. It’s not about how you feel. It’s about stopping damage before it starts.
Can I travel after a kidney transplant?
Yes, but plan carefully. Avoid areas with poor sanitation or outbreaks of diseases like dengue or malaria. Carry your medication list, know where the nearest transplant center is, and avoid raw food and untreated water. Talk to your team before booking any trip. Some destinations require vaccines you can’t get after transplant.
What’s the biggest mistake transplant patients make?
Thinking they’re "out of the woods" after six months. Most infections happen after the first year. Stopping precautions too soon-like skipping handwashing, eating risky foods, or skipping vaccines-is the leading cause of preventable illness. Your transplant is a long-term commitment to safety.
Post-transplant infections aren’t inevitable. They’re preventable. With the right vaccines, medicines, daily habits, and monitoring, you can live a full, active life with your new kidney. The science is clear. The tools are here. Now it’s up to you.
Comments (8)