Most people know psoriasis as that stubborn, scaly skin condition - red patches on elbows, knees, or scalp that won’t quit. But what many don’t realize is that for about 30% of those with psoriasis, the problem doesn’t stop at the skin. The same immune system that attacks the skin starts attacking the joints, leading to psoriatic arthritis. This isn’t just a coincidence. It’s a direct link. And if you’ve been ignoring joint stiffness, swollen fingers, or achy heels while focusing only on your skin, you could be missing the early warning signs.
It’s Not Just Dry Skin - It’s an Inside Job
Psoriatic arthritis doesn’t appear out of nowhere. It’s the body’s immune system going rogue. In psoriasis, immune cells mistakenly target skin cells, causing them to grow too fast and pile up into plaques. In psoriatic arthritis, those same immune cells turn their attention to the joints, tendons, and even the places where tendons attach to bone. This isn’t wear-and-tear like osteoarthritis. This is active inflammation - the kind that can destroy cartilage and bone if left unchecked.What makes this tricky is timing. For most people, skin symptoms come first - usually 5 to 10 years before joint pain starts. But in about 15% of cases, the joints hurt before the skin shows any signs. That’s why so many people end up seeing three or more doctors before getting the right diagnosis. One Reddit user, 'PsOandMe,' shared how they had 18 months of worsening joint pain before their rheumatologist connected their nail pitting to their skin patches. By then, permanent damage had already set in.
What Does Psoriatic Arthritis Actually Feel Like?
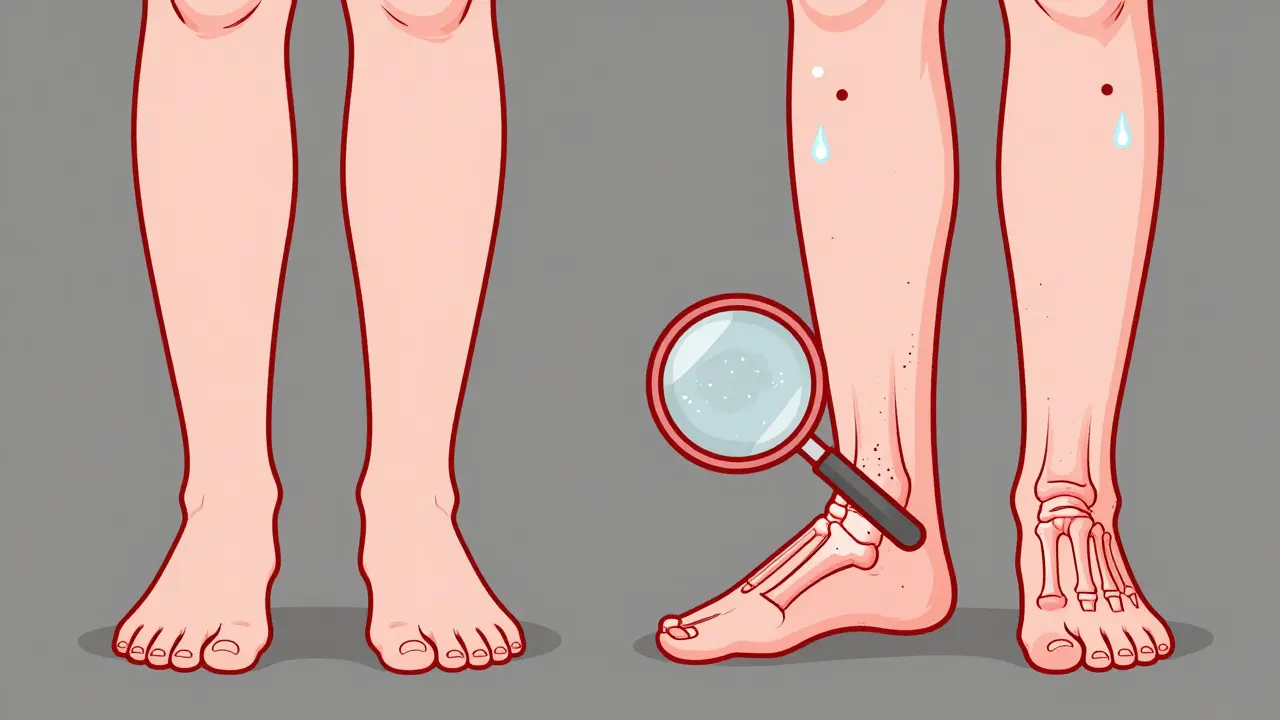
The symptoms aren’t just "aches and pains." They’re specific, telling, and often overlooked.- Sausage digits (dactylitis): One or more fingers or toes swell up completely - not just the joint, but the whole digit. It looks like a little sausage. This happens in 40-50% of people with psoriatic arthritis and is rare in other types of arthritis.
- Enthesitis: Pain where tendons or ligaments meet bone. Think Achilles tendon pain in the back of the heel or pain under the foot (plantar fasciitis). About 35-50% of patients experience this, and it’s often mistaken for overuse or sports injury.
- Nail changes: Pitting, separation from the nail bed, or yellow-brown discoloration. Eighty percent of people with psoriatic arthritis who have nail issues show these signs. If you’ve had pitted nails for years and now your knuckles hurt, that’s a red flag.
- Morning stiffness: Not just any stiffness - this lasts more than 30 minutes and doesn’t improve with light movement. It’s often worse after sitting still, like after a long drive or sleeping.
And here’s something many don’t expect: psoriatic arthritis can also cause eye redness (uveitis) or digestive issues like Crohn’s disease. It’s not just a joint disease. It’s a whole-body condition.
Five Types - Not Just One
Psoriatic arthritis doesn’t show up the same way for everyone. There are five distinct patterns, and knowing which one you have helps guide treatment.- Asymmetric oligoarthritis: The most common type - affects fewer than five joints, and not the same ones on both sides. For example, your left wrist and right knee. About 35-40% of cases.
- Symmetric polyarthritis: Looks like rheumatoid arthritis - same joints on both sides. But unlike RA, it doesn’t usually test positive for rheumatoid factor. Affects 25-30%.
- Distal interphalangeal predominant (DIP): Targets the joints closest to the fingernails. Rare in other arthritic conditions. Often linked to severe nail changes. Seen in about 25% of cases.
- Spondylarthritis: Involves the spine and sacroiliac joints. Causes lower back pain that improves with movement - the opposite of mechanical back pain. Affects 5-10%.
- Arthritis mutilans: The rarest and most destructive. Causes bone loss, leading to shortened fingers or toes - sometimes called "opera glass hand." Happens in less than 5%.
Getting the subtype right matters. If you have spondylarthritis, you need different imaging and monitoring than someone with dactylitis. One size doesn’t fit all.
How Is It Different From Other Arthritides?
It’s easy to confuse psoriatic arthritis with other joint diseases. Here’s how to tell them apart:| Feature | Psoriatic Arthritis | Rheumatoid Arthritis | Osteoarthritis |
|---|---|---|---|
| Joint Pattern | Often asymmetric | Almost always symmetric | Asymmetric, weight-bearing joints |
| Rheumatoid Factor | Negative | Positive in 80% | Negative |
| Enthesitis | Common (35-50%) | Rare | Not present |
| Dactylitis | Common (40-50%) | Very rare | Not present |
| Nail Changes | Very common (80%) | Uncommon | Not related |
| Imaging Findings | Pencil-in-cup erosions, new bone growth | Uniform joint space loss | Bone spurs, cartilage thinning |
| Systemic Inflammation | Yes - affects skin, eyes, gut | Yes - affects lungs, heart | No - local wear and tear |
That’s why a simple blood test isn’t enough. You need a doctor who looks at your skin, your nails, your feet, your back - not just your hands.
Why Early Diagnosis Is Critical
The biggest danger? Delay. The longer you wait, the more damage you risk.Studies show that if you’re diagnosed more than six months after symptoms start, your chance of permanent joint damage jumps dramatically. One Toronto study found that people with delays over 12 months had 3.2 times more bone erosion at five years than those diagnosed early.
And it’s not just about mobility. Psoriatic arthritis increases your risk of heart disease by 2.1 times and diabetes by 1.8 times - because chronic inflammation doesn’t stay in the joints. It spreads.
Doctors now use tools like the MASES score (for enthesitis), Dactylitis Count, and NAPSI (Nail Psoriasis Severity Index) to track progress. These aren’t just checklists - they’re early warning systems.
What Works - And What Doesn’t
Treatment has changed dramatically in the last decade. It’s no longer just about painkillers.- DMARDs like methotrexate: Used in 65% of new cases. Helps slow damage but doesn’t always control inflammation well.
- TNF inhibitors (e.g., adalimumab, etanercept): Prescribed for 45% of moderate to severe cases. Work well for skin and joints. About 65% of patients reach minimal disease activity within six months.
- IL-17 and IL-23 inhibitors (e.g., secukinumab, guselkumab): Newer, faster-acting. The FUTURE 7 trial showed guselkumab achieved 64% improvement in joint symptoms at 24 weeks - far better than placebo.
- JAK inhibitors: Effective, but carry a higher risk of heart events and cancer. The FDA requires special monitoring for these.
Here’s the hard truth: about 30% of people don’t respond well to their first biologic. That’s why treatment is personal. Your doctor may need to try two or three drugs before finding the right one.
Triggers and Lifestyle - What You Can Control
You can’t change your genes. But you can change what pushes your symptoms into flare mode.- Stress: Cited by 85% of patients as a major trigger. Meditation, therapy, or even daily walks can help.
- Infections: Strep throat can spark a flare. Treat infections fast.
- Cold weather: 57% of patients report worse symptoms in winter. Keep joints warm.
- Obesity: A BMI over 30 increases your risk of psoriatic arthritis by 2.3 times. Losing even 10% of body weight improves joint pain and skin symptoms.
- Alcohol and smoking: Both worsen inflammation and reduce treatment effectiveness.
There’s no magic diet, but cutting processed foods and sugar helps. Many patients report less swelling and better energy on anti-inflammatory diets - even without clinical proof.
Coordinated Care Is Non-Negotiable
This isn’t a dermatology problem or a rheumatology problem. It’s both.Research shows that when dermatologists and rheumatologists work together, 82% of patients achieve good outcomes. When they don’t - only 54% do.
That means: if you’re seeing a dermatologist for your skin, ask them: "Could this be psoriatic arthritis?" If you’re seeing a rheumatologist for joint pain, ask: "Do I have psoriasis or nail changes?" Don’t wait for them to connect the dots. Be the one who brings it up.
What’s Next?
The future is personalized. By 2027, doctors will likely use genetic and protein markers to predict which drug will work best for you - before you even take it. Clinical trials are exploring JAK inhibitors, new IL blockers, and even therapies that reset immune cells.But right now, the most powerful tool you have is awareness. If you have psoriasis and you’re feeling stiff, swollen, or achy - don’t brush it off. Don’t assume it’s aging. Don’t wait for your next skin appointment.
See a rheumatologist. Get imaging. Track your symptoms. And remember: your skin isn’t the only thing that matters. Your joints are screaming - listen to them.
Can psoriatic arthritis happen without skin psoriasis?
Yes, but it’s uncommon. About 15% of people develop joint symptoms before any visible skin psoriasis appears. This makes diagnosis harder, because doctors may not suspect psoriatic arthritis without the classic skin plaques. Nail changes, dactylitis, or enthesitis in someone with a family history of psoriasis should raise suspicion even without visible skin disease.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. While both cause joint inflammation, rheumatoid arthritis is symmetric (affects both sides equally), tests positive for rheumatoid factor, and rarely involves the spine or entheses. Psoriatic arthritis is often asymmetric, is rheumatoid factor negative, and commonly affects the nails, entheses, and spine. The treatment approaches overlap but aren’t identical - some drugs work better for one than the other.
Can psoriatic arthritis be cured?
There’s no cure yet, but it can be controlled. With early treatment using biologics or targeted therapies, many people reach minimal disease activity - meaning little to no pain, swelling, or damage progression. The goal isn’t to eliminate the disease, but to stop it from damaging your joints and organs. Many patients live full, active lives with proper management.
What’s the best test to diagnose psoriatic arthritis?
There’s no single blood test. Diagnosis combines clinical signs (nail changes, dactylitis, enthesitis), imaging (X-rays or MRI showing bone changes like pencil-in-cup erosions or new bone growth), and ruling out other conditions. The 2023 ACR/EULAR classification criteria now include imaging and biomarker patterns, improving accuracy to 92%. A rheumatologist will look at your full picture - not just one result.
Does psoriatic arthritis get worse with age?
Not necessarily because of age, but because of how long it’s been untreated. The disease itself doesn’t automatically worsen over time - but inflammation does. Without treatment, joint damage accumulates. That’s why early intervention is so critical. Someone diagnosed at 35 and treated well may have no progression by 60. Someone untreated for 10 years may face severe disability regardless of age.
Can I still exercise with psoriatic arthritis?
Yes - and you should. Movement reduces stiffness, strengthens muscles around joints, and lowers inflammation. Low-impact activities like swimming, cycling, yoga, and walking are ideal. Avoid high-impact sports during flares. Physical therapy can help tailor a safe routine. Many patients report that regular movement is more effective for morning stiffness than medication.
Do biologics have serious side effects?
They can. Biologics suppress parts of the immune system, so you’re more vulnerable to infections like tuberculosis or fungal infections. JAK inhibitors carry a higher risk of heart events and cancer, which is why the FDA requires special monitoring. But for most people, the benefits outweigh the risks - especially compared to the damage uncontrolled psoriatic arthritis causes. Regular blood tests and screenings help manage these risks.

Comments (12)