When your face turns red without warning-after a cup of coffee, a spicy meal, or even just walking outside-it’s more than just blushing. For millions of people, this is rosacea, a stubborn skin condition that doesn’t go away with regular skincare. It starts with flushing, then settles into persistent redness, bumps, and visible blood vessels. And while it can’t be cured, it can be managed. One of the most common and effective ways? Topical antibiotics.
What Rosacea Really Looks Like
Rosacea isn’t acne. It’s not just sensitive skin. It’s a chronic inflammatory condition that mostly hits the central face: cheeks, nose, chin, and forehead. You might notice it first as sudden redness that comes and goes. That’s facial flushing-the earliest sign in about 75% of cases. Unlike normal blushing, which fades in minutes, rosacea flushing can last for hours. It’s often triggered by heat, alcohol, spicy food, sun exposure, or even stress.
Over time, the redness becomes permanent. Blood vessels widen and stay dilated, creating a web of fine red lines. Then come the bumps-tiny pimples that aren’t caused by dirt or oil. These are inflammatory lesions, and they’re what make people feel self-conscious. About 50% of those with rosacea develop this papulopustular subtype. And it’s not just skin deep: nearly half of patients report anxiety or depression because of how it looks.
There’s also a lesser-known side: eye irritation. Around half of rosacea patients get dry, gritty, burning eyes. It’s called ocular rosacea, and it’s often overlooked. If your eyes feel like they’re full of sand, it might be linked to the redness on your face.
Why Topical Antibiotics? Not What You Think
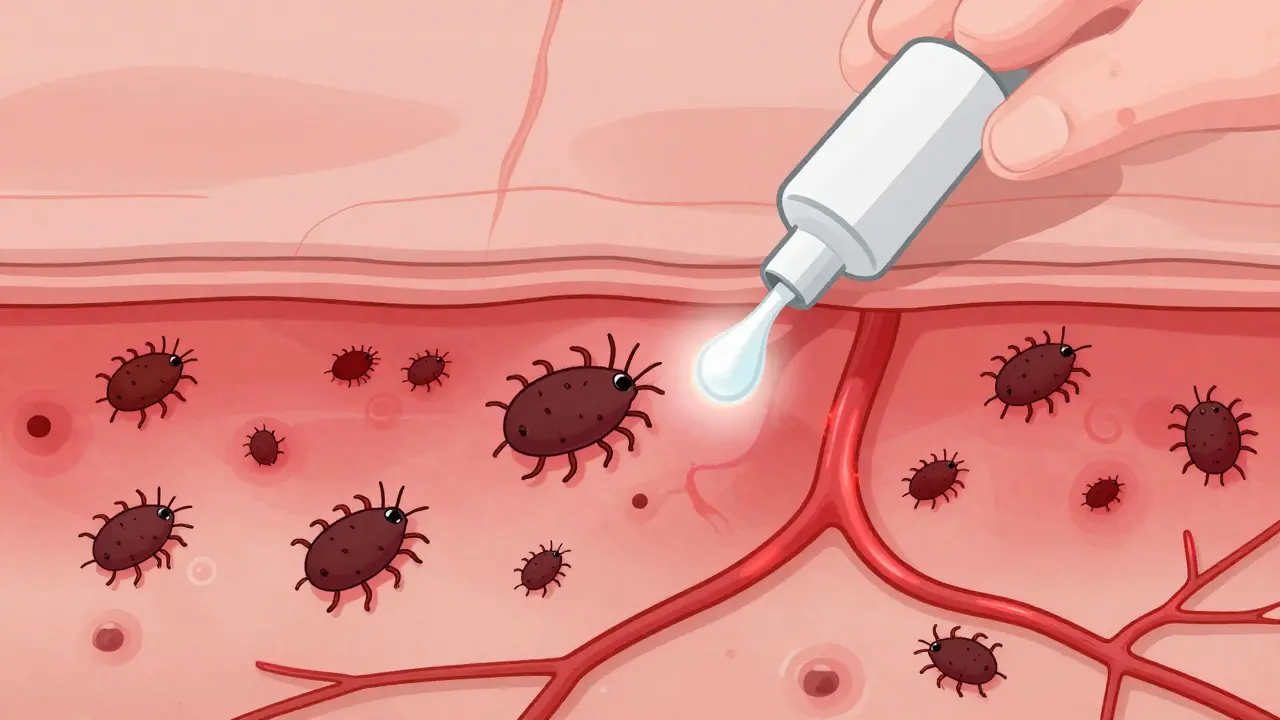
When you hear "antibiotic," you might think of fighting infection. But with rosacea, it’s not about killing bacteria. It’s about calming inflammation. The skin’s immune system goes into overdrive, and tiny mites called Demodex folliculorum-normally harmless-may be triggering the reaction. Topical antibiotics work by reducing this inflammation and suppressing the immune response in the skin.
Three main topical antibiotics are used today: metronidazole, ivermectin, and azelaic acid. All are applied as gels or creams once or twice daily. None are cures. But they can turn a flare-up into something manageable.
Metronidazole: The Longtime Standard
Metronidazole 0.75% gel (sold as Rozex®) has been the go-to for decades. It was approved by the FDA in 1985 and still works well for many. Clinical trials show it reduces inflammatory bumps and pimples by 60-70% after 6 to 9 weeks of use. It’s gentle, affordable, and ideal for sensitive skin. About 15% of users feel a slight sting at first, but that usually fades.
It’s not flashy. But it’s reliable. Many dermatologists start with metronidazole, especially if the skin is already irritated. It’s also the most common choice for people who can’t afford newer treatments.
Ivermectin: The New Gold Standard
Ivermectin 1% cream (Soolantra®) came onto the scene in 2014 and quickly changed the game. In a major 2019 study published in the New England Journal of Medicine, it reduced lesions by 76% after 12 weeks-compared to just 55% with metronidazole. That’s a 22% improvement, and it’s statistically significant.
Why does it work better? It doesn’t just calm inflammation. It also targets Demodex mites, which are found in higher numbers on rosacea-prone skin. One user on Reddit shared, "After 8 weeks of Soolantra, my facial bumps reduced by 80% with minimal irritation." That’s not rare. In fact, 62% of users on Drugs.com rate it positively.
It’s more expensive than metronidazole. But for many, the results justify the cost. Dermatologists now often recommend it as a first-line treatment for moderate to severe papulopustular rosacea.
Azelaic Acid: The Non-Antibiotic Option
Azelaic acid 15% gel (Finacea®) isn’t technically an antibiotic, but it’s often grouped with them because it treats the same symptoms. It reduces redness and bumps by 68-73% after 15 weeks. It’s especially helpful for people who get irritated by other treatments. It also works on dark spots and uneven texture.
The downside? It takes longer. You need to stick with it for at least 3 months to see the full effect. And some users report stinging, especially if they apply it on damp skin. But if you’re looking for something that also improves overall tone, it’s a solid pick.
What You Need to Know Before Starting
Topical antibiotics don’t work overnight. Expect to wait 4 to 8 weeks just to notice a difference. Full results take 12 to 16 weeks. That’s hard to accept when your face is burning and red. Many people quit too soon.
Here’s what actually works:
- Use a pea-sized amount for your entire face. Too much causes irritation.
- Apply it to completely dry skin, at least 15 minutes after washing.
- Don’t layer it over other actives like retinoids or acids. Stick to gentle cleansers and mineral sunscreen (zinc oxide 10-20%).
- Do a patch test on your jawline for 3 days before using it all over.
Side effects are usually mild: dryness, stinging, or slight redness. Less than 1% of users have serious reactions. If your skin gets worse in the first two weeks, don’t panic. That’s common. Stick with it unless it becomes unbearable.
What These Treatments Don’t Do
Here’s the hard truth: topical antibiotics don’t fix facial flushing. They don’t shrink blood vessels. They don’t erase persistent redness. That’s why many people still look red even after their bumps are gone.
If flushing is your main problem, you might need something else. Brimonidine gel (Mirvaso®) and oxymetazoline cream (Rhofade®) temporarily constrict blood vessels. They’re fast-acting but meant for short-term use. They’re not replacements-they’re partners.
And don’t forget triggers. If you keep drinking red wine, eating spicy food, or skipping sunscreen, no cream will fully work. Keeping a symptom diary helps. Note what you ate, where you were, and how red your face got. Patterns emerge.
Real-Life Challenges
Cost is a big barrier. Without insurance, these creams can cost $350 a year. That’s why many people stop after a few months. Some turn to generic versions, but not all are equally effective.
Adherence is the biggest hurdle. Studies show only 40-50% of people keep using their medication beyond 3 months. Why? Slow results. Skin irritation. The feeling that it’s not "working." But if you’ve made it this far, know this: improvement is cumulative. The redness fades slowly. The bumps disappear one by one. It’s not dramatic-but it’s real.
And don’t go it alone. The National Rosacea Society has a directory of over 1,200 dermatologists who specialize in this. Telehealth services like Curology offer consultations starting at $45/month. You don’t need to suffer in silence.
The Future of Treatment
The rosacea treatment market is growing fast. Topical therapies now make up 65% of it. Ivermectin has overtaken metronidazole as the most prescribed. And new combinations are on the horizon. Galderma’s 2023 trials show a cream with ivermectin and hydrocortisone reduces lesions by 85%-better than either alone.
But the core remains the same: gentle care, consistent treatment, and patience. There’s no magic bullet. But there are proven tools. And with the right approach, many people go from hiding their faces to feeling confident again.
Can topical antibiotics cure rosacea?
No, topical antibiotics cannot cure rosacea. Rosacea is a chronic condition with no known cure. These treatments help manage symptoms-especially inflammatory bumps and pimples-but they don’t stop facial flushing or eliminate persistent redness. Long-term management, including trigger avoidance and skincare, is essential.
How long does it take for topical antibiotics to work?
Most people start noticing improvement after 4 to 8 weeks of daily use. Full results typically take 12 to 16 weeks. This slow progress is why many patients stop too early. Consistency is key-skip doses, and you’ll delay results.
Is ivermectin better than metronidazole?
Yes, for most people with moderate to severe papulopustular rosacea. A 2019 study showed ivermectin reduced lesions by 76% compared to 55% with metronidazole. Ivermectin also targets Demodex mites, which may play a role in triggering inflammation. However, metronidazole is gentler on sensitive skin and more affordable, making it a good first option for some.
Do I need to use sunscreen with topical antibiotics?
Absolutely. Sun exposure is one of the top triggers for rosacea flushing and worsening redness. Use a mineral sunscreen with zinc oxide (10-20%) every day, even when it’s cloudy. Avoid chemical sunscreens-they can sting sensitive rosacea skin.
Can I use makeup while on topical antibiotics?
Yes, but choose wisely. Use non-comedogenic, fragrance-free, mineral-based makeup. Apply your topical treatment first, wait 15 minutes, then apply makeup. Avoid heavy foundations-they can clog pores and trap heat, making flushing worse. Green-tinted color correctors can help mask redness temporarily.
