SGLT2 Inhibitor Risk Assessment Tool
Assess Your Risk
This tool helps you understand your risk of dehydration and dizziness when taking SGLT2 inhibitors based on your health factors.
Your Risk Assessment
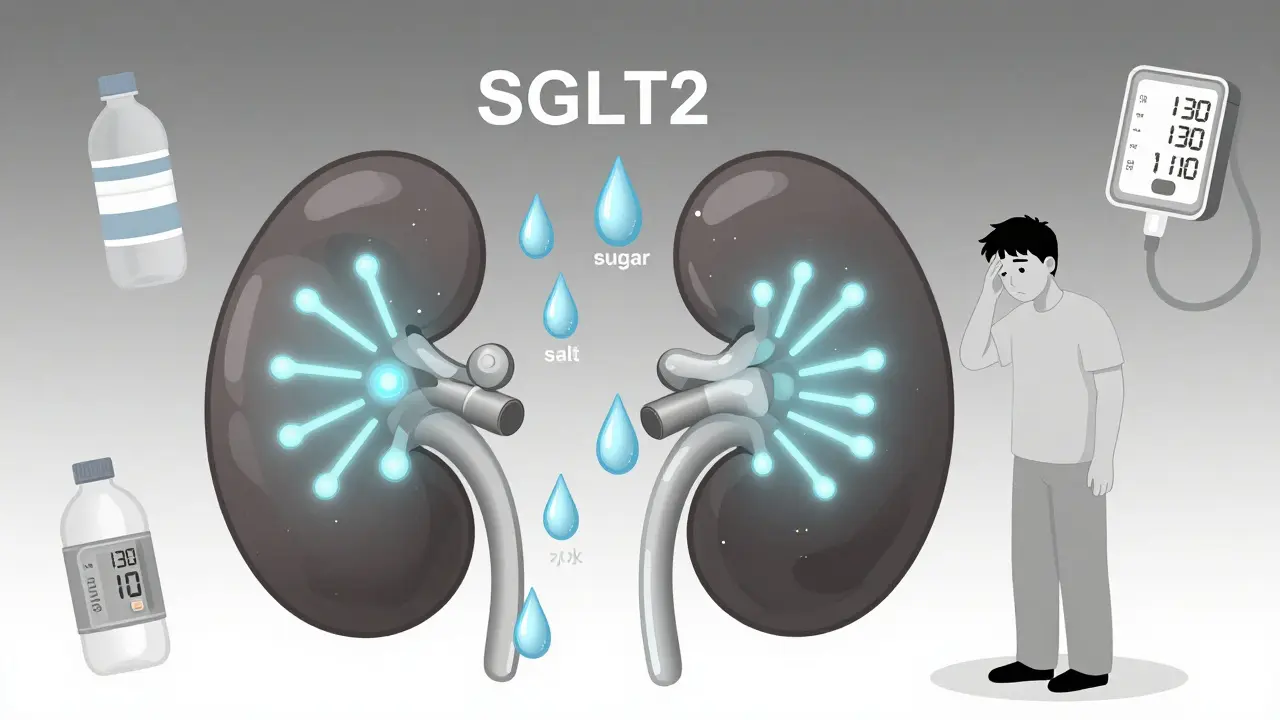
When you start taking an SGLT2 inhibitor for type 2 diabetes, you might not expect to feel dizzy or unusually thirsty. But these side effects aren’t rare - they’re built into how the drug works. SGLT2 inhibitors like empagliflozin (a medication that lowers blood sugar by making the kidneys flush out excess glucose and sodium), dapagliflozin, and canagliflozin aren’t just sugar-lowering pills. They act like mild diuretics, pulling water and salt out of your body through urine. That’s why they help your heart and kidneys - but it’s also why some people feel lightheaded, dry-mouthed, or even faint.
How SGLT2 Inhibitors Work: More Than Just Lowering Sugar
These drugs block a protein in your kidneys called SGLT2, which normally reabsorbs glucose back into your blood. When it’s blocked, about 70 to 100 grams of sugar leak out in your urine every day. That’s like throwing away 250 to 400 calories daily - no exercise needed. But here’s the catch: when glucose leaves, it drags sodium and water with it. Your kidneys end up producing more urine, not because you drank more, but because your body is literally flushing out sugar and salt.
This isn’t just about blood sugar. Studies show SGLT2 inhibitors reduce systolic blood pressure by 4 to 6 mmHg on average within two weeks. That’s similar to the effect of a low-dose diuretic. The drop happens because less fluid in your bloodstream means less pressure on your artery walls. At the same time, your arteries relax slightly due to improved blood vessel function. That’s why these drugs are now recommended for heart failure - even in people without diabetes.
Why You Might Feel Dehydrated
Dehydration from SGLT2 inhibitors isn’t about not drinking enough water. It’s about your body losing more fluid than usual. Clinical trials report that 1.3% to 2.8% of users experience volume depletion - symptoms like dry mouth, dark urine, fatigue, or reduced urination. Older adults are at higher risk: people over 65 are 2.1 times more likely to have dehydration-related hospital visits than younger users. Why? Because older bodies don’t sense thirst as well, and many are already on blood pressure meds that also reduce fluid.
Patients with kidney problems (eGFR under 60 mL/min) are especially vulnerable. When your kidneys are already struggling, adding a drug that pushes even more fluid out can tip the balance. In the CANVAS trial, canagliflozin nearly doubled the risk of volume depletion in patients with moderate kidney disease. If you’re on a loop diuretic like furosemide, the combo can be too much. One patient on Reddit shared: “Canagliflozin made me so dehydrated I had to stop after 3 weeks - constant thirst but dry mouth.”
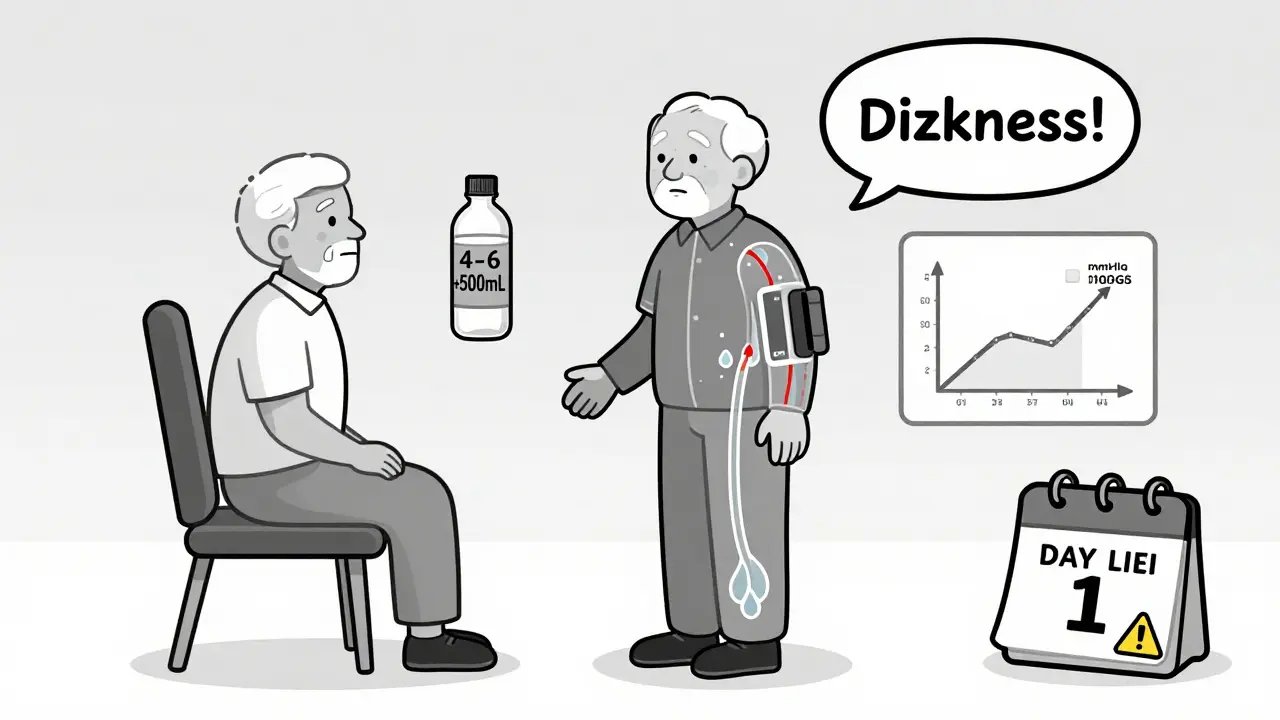
Dizziness: It’s Not Just in Your Head
Dizziness is one of the most common complaints. Clinical data shows 3.5% to 5.8% of users report it - compared to just 2.5% to 3.2% on placebo. But it’s rarely random. About 63% of dizziness cases are tied to orthostatic hypotension - meaning your blood pressure drops when you stand up. This happens because your body hasn’t adjusted yet to the lower fluid volume.
Most cases show up in the first four weeks. The FDA tracked over 2,800 dizziness reports from 2013 to 2022. Canagliflozin had the highest rate - 6.3 cases per 1,000 patient-years. Why? It’s the strongest diuretic in the class. Dizziness isn’t dangerous for most people - it usually fades as your body adapts. But for older adults, those on multiple blood pressure pills, or those with baseline systolic pressure under 130 mmHg, the risk is real. One study found that patients with systolic pressure below 130 had nearly three times the odds of dizziness.
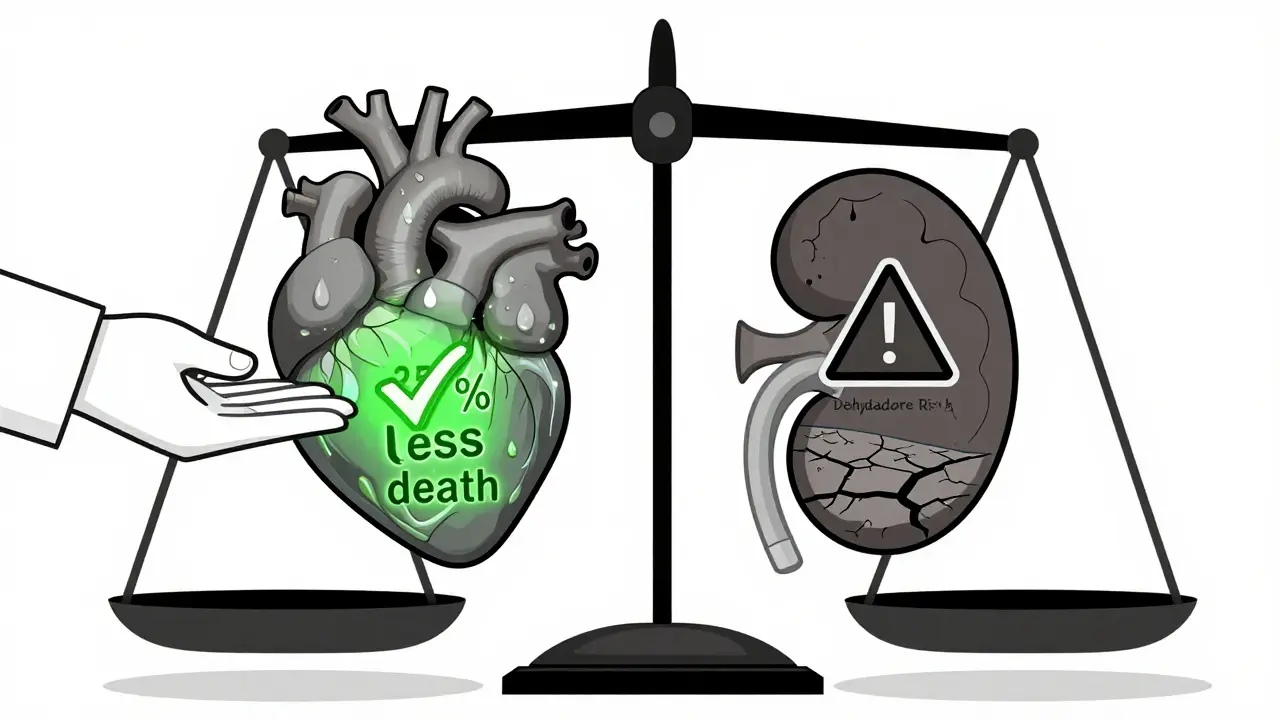
Blood Pressure Drops - and Why That’s Actually Good (Most of the Time)
Yes, SGLT2 inhibitors lower blood pressure. But that’s not a bug - it’s a feature. In heart failure patients, even a 5 mmHg drop can mean fewer hospital visits and longer life. The EMPEROR-Reduced trial showed empagliflozin cut cardiovascular death by 25% in heart failure patients. The DAPA-HF trial found dapagliflozin reduced death from heart failure by 17% over 18 months. That’s 6 lives saved per 100 patients.
But here’s the tension: the same mechanism that helps your heart can hurt your balance. If your blood pressure was already low - say, under 120 mmHg - you’re 3.2 times more likely to have symptoms like fainting or dizziness. That’s why doctors now check orthostatic blood pressure before starting these drugs. If your pressure drops more than 20 mmHg systolic when you stand, they’ll pause the medication until you’re stable.
Who’s at Risk - And What to Do
You’re at higher risk if:
- You’re over 65
- You have kidney disease (eGFR under 60)
- You’re on other diuretics or ACE inhibitors
- Your blood pressure is consistently below 130 mmHg
- You’re sick with vomiting, diarrhea, or a fever
Here’s what you can do:
- Drink more water - add 500 to 1,000 mL daily when you start, especially in hot weather.
- Stand up slowly - give your body time to adjust.
- Monitor your weight - a 1.5 to 2.5 kg drop in the first week is normal. If you lose more than 3 kg in a week, call your doctor.
- Check your blood pressure - if it drops below 90 mmHg systolic, pause the drug until you’re rehydrated.
- Don’t skip follow-ups - most doctors want to see you within 7 to 10 days after starting.
Many patients stop the drug because of dizziness. But experts say: don’t quit too soon. In most cases, the side effects fade within a month. If they don’t, your doctor can reduce the dose - like switching from 25 mg empagliflozin to 10 mg - instead of stopping entirely. The cardiovascular benefits often outweigh the temporary discomfort.
What Patients Really Say
On Drugs.com, 38.7% of empagliflozin users report dizziness. But 62% say it was mild and went away. On Reddit, one user wrote: “Started Jardiance last week and got dizzy standing up - my doctor said it’s normal for the first month.” Another said: “I lost 5 pounds in 10 days - I thought I was losing fat. Turns out, I was losing fluid.”
Doctors agree: education is key. A 2022 survey of endocrinologists found 84% check for orthostatic changes at the first follow-up. Nearly half reduce the dose instead of stopping. The message is clear: these side effects are manageable. They’re not a reason to avoid the drug - they’re a reason to use it wisely.
Final Thoughts
SGLT2 inhibitors are changing how we treat diabetes, heart failure, and kidney disease. But they’re not magic pills. They work by changing how your body handles fluid - and that has real consequences. Dehydration and dizziness aren’t side effects you can ignore. But they’re also not reasons to panic. With smart monitoring, a little extra water, and careful timing, most people can get the benefits without the discomfort.
If you’re on one of these drugs and feel lightheaded, don’t assume it’s just aging. Talk to your doctor. Check your blood pressure. Drink more. Wait it out. And remember: what feels like a problem today might be the very thing that saves your heart tomorrow.
Can SGLT2 inhibitors cause serious dehydration?
Yes, but it’s uncommon. Clinical trials show 1.3% to 2.8% of users experience volume depletion symptoms like dry mouth, fatigue, or reduced urination. Risk is highest in older adults, those with kidney disease, or those on other diuretics. Hospitalization for dehydration occurs in about 0.8% of users, compared to 0.4% on placebo. Staying hydrated and avoiding illness can prevent most cases.
Why do SGLT2 inhibitors make me dizzy?
Dizziness is usually caused by orthostatic hypotension - a sudden drop in blood pressure when standing. SGLT2 inhibitors reduce fluid volume and lower blood pressure, which can cause your brain to get less blood temporarily. This happens most often in the first 4 weeks. About 63% of dizziness cases are linked to this mechanism. The risk is higher if you’re over 75, have low blood pressure, or take other blood pressure medications.
Do SGLT2 inhibitors lower blood pressure too much?
They lower blood pressure by 4-6 mmHg systolic on average - which is beneficial for most people, especially those with heart failure or high blood pressure. But if your blood pressure was already low (below 120 mmHg), you’re at higher risk of symptoms like fainting or dizziness. Doctors recommend checking orthostatic blood pressure before starting and again after one week. If systolic pressure drops below 90 mmHg, the drug may need to be paused.
Should I stop taking SGLT2 inhibitors if I feel dizzy?
Not necessarily. Dizziness often fades within 2-4 weeks as your body adjusts. Instead of stopping, try drinking more water, standing up slowly, and checking your blood pressure. If symptoms persist, your doctor may reduce the dose - for example, from 25 mg to 10 mg of empagliflozin - rather than stopping completely. The cardiovascular benefits usually outweigh the temporary side effects.
Are SGLT2 inhibitors safe for elderly patients?
Yes, but with caution. Older adults are more likely to experience dehydration and dizziness due to reduced thirst sensation and higher rates of kidney decline. Studies show they’re 2.1 times more likely to be hospitalized for volume depletion. Starting with a lower dose, increasing fluid intake, and monitoring weight and blood pressure weekly can make these drugs safe and effective even in patients over 75.
Can I take SGLT2 inhibitors if I’m on a diuretic?
Yes, but your doctor will likely adjust the dose. Combining SGLT2 inhibitors with loop diuretics like furosemide increases the risk of dehydration and low blood pressure. In clinical practice, doctors often reduce the diuretic dose by 25-50% when starting an SGLT2 inhibitor. Never change doses on your own - always consult your provider first.
Comments (15)