Expiration dates on medicine bottles and food packages aren’t just random numbers. They’re the result of months - sometimes years - of rigorous science designed to answer one question: When does this product stop being safe and effective? For generic drugs and everyday food items, the stakes are high. A pill that loses potency, a sauce that grows mold, or a cream that separates isn’t just inconvenient - it can be dangerous. Yet many people assume that if it looks fine and the date hasn’t passed, it’s still good. That’s a dangerous assumption.
What Stability Testing Really Measures
Stability testing isn’t about watching a product sit on a shelf. It’s a controlled, scientific process that tracks how a product changes over time under specific conditions. The U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) require this for all pharmaceuticals. The same standards apply to many food products, especially those with preservatives or sensitive ingredients. There are four key areas tested:- Chemical stability: Does the active ingredient break down? For example, levothyroxine, a common thyroid medication, can degrade if exposed to moisture. A 2020 FDA study found 17.3% of generic versions had stability issues not seen in the brand-name version, Synthroid - all because of differences in how the packaging protected against humidity.
- Physical stability: Does it still look and feel right? Pills might crumble, liquids might cloud, creams might separate. For nanoparticle-based drugs - like those used in cystic fibrosis treatments - particles must stay under 200 nanometers. If they clump together beyond that, they can’t reach the target cells, making the drug useless.
- Microbiological stability: Is it still free from harmful bacteria or mold? Non-sterile products like eye drops or oral suspensions must stay below 100 colony-forming units per gram (CFU/g). If preservatives break down over time, even a product that looks clean can become a breeding ground for pathogens.
- Functional stability: Does it still work as designed? An inhaler must deliver the exact dose each time. If the propellant degrades or the valve clogs, the patient gets too little - or too much - medicine.
These aren’t optional checks. They’re legally required. Under 21 CFR 211.166, manufacturers must prove their product stays within these limits for the entire shelf life listed on the label.
The Myth of Accelerated Testing
To save time, companies often use accelerated testing: storing a product at high heat (40°C) and humidity (75%) for six months to predict what will happen over two years. It sounds smart - until it fails. A quality assurance professional on the American Pharmaceutical Review forum shared a costly mistake: their team ran accelerated tests at 40°C and saw no degradation. They approved a 24-month shelf life. But in real-world storage at room temperature, the product crystallized at the 24-month mark. They lost $250,000 and 18 months of work. Why? Because high heat can trigger a completely different degradation pathway than room temperature. A chemical reaction that happens slowly over years might not even occur under fast stress. Or worse - it might skip a step and create a new, harmful byproduct. The ICH Q1A(R2) guidelines allow companies to extrapolate shelf life beyond the tested period - but only if changes are minimal and scientifically justified. Too many companies treat this as a loophole, not a responsibility. The FDA’s 2022 inspection guide warns that “performing accelerated testing at very high temperatures for a very short time and expecting to extrapolate results to a very long expiration dating period” is scientifically flawed.Why Generic Drugs Are a Special Case
Generic drugs are cheaper because they don’t repeat expensive clinical trials. But they still must prove bioequivalence - meaning they deliver the same amount of active ingredient to the body as the brand-name version. What they don’t have to prove is identical stability. Generics often use different fillers, binders, or coatings. These “excipients” can affect how moisture, light, or heat interacts with the active drug. A 2020 FDA report showed that generic levothyroxine products with inferior moisture barriers degraded faster than Synthroid. Patients taking these versions risked underdosing - leading to fatigue, weight gain, and even heart problems. Even small differences in manufacturing can matter. One company might use a tablet press that creates a denser pill, slowing moisture absorption. Another might use a cheaper film coating that cracks under humidity. Neither is illegal - but both can affect shelf life. And here’s the catch: patients often switch between generic brands without knowing. One month, they get a pill from Manufacturer A. The next, from Manufacturer B. If those two have different stability profiles, the patient’s dose fluctuates - sometimes dangerously.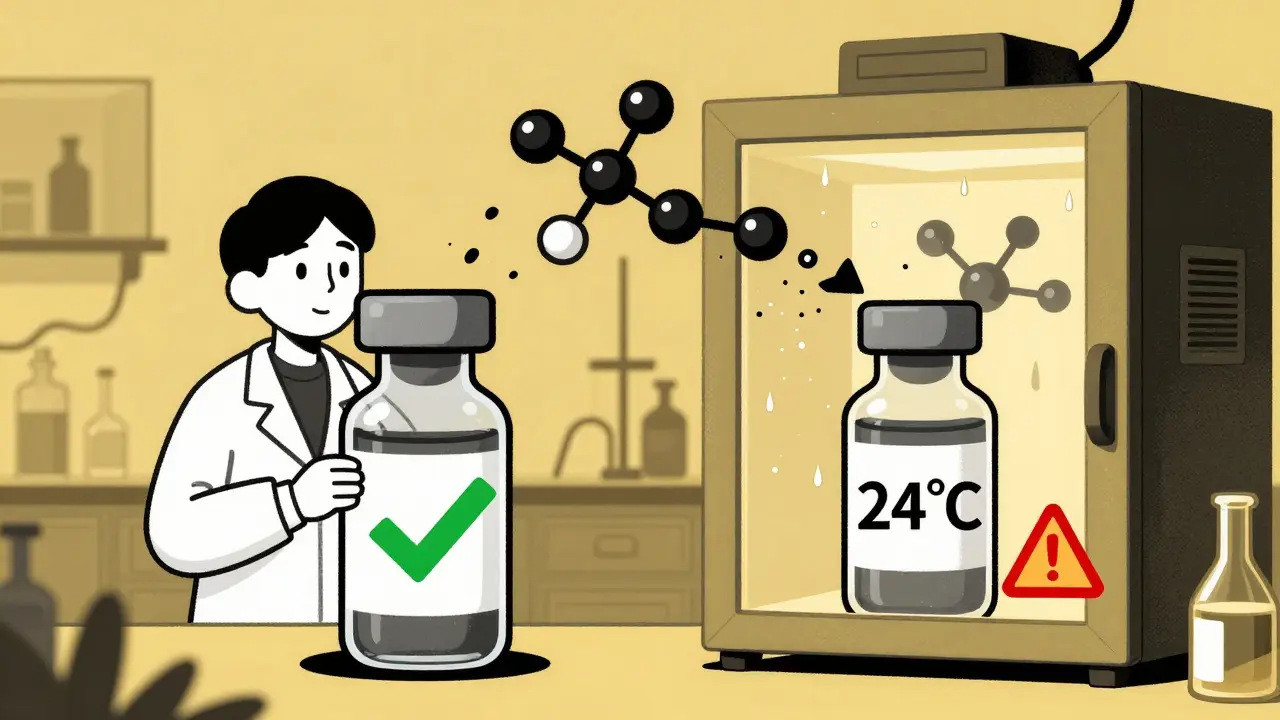
Storage Conditions Matter More Than You Think
You’ve seen the label: “Store at room temperature.” But what does that mean? The FDA defines “room temperature” as 15-30°C (59-86°F). But research shows 24-25°C is the real benchmark for stability studies. That’s not the same as “inside your medicine cabinet.” In many homes, medicine cabinets sit above sinks or near windows. Heat and humidity rise. In Cape Town, where summer temperatures regularly hit 32°C, a bathroom cabinet can easily reach 35°C. That’s outside the approved range. The FDA issues warning letters for this. In fact, 80% of stability-related citations on FDA Form 483s are for poor storage documentation. Saying “room temperature” isn’t enough. You need to show you monitored actual conditions - with data loggers, temperature logs, and humidity controls. Even the packaging matters. A blister pack might protect a pill from air, but not from moisture. A brown glass bottle might block light, but not humidity. A bottle with a cotton plug? That’s a moisture trap.What Happens When Stability Fails
When a product degrades, it doesn’t just become weaker. It can become toxic. In 2018, a batch of generic ranitidine (Zantac) was recalled after testing revealed the formation of NDMA - a known carcinogen - as the drug broke down over time. The compound wasn’t present when the product was made. It formed during storage. In food, microbial growth isn’t always visible. A yogurt with low preservative levels might look fine but harbor Listeria. A jar of pickles with a compromised seal might develop botulism - odorless, tasteless, and deadly. The Parenteral Drug Association found that 41.3% of stability-related recalls in the last five years were due to microbial growth from changes in water activity. That’s not contamination from the factory - it’s degradation over time. And the consequences aren’t just health risks. A single recall can cost a company millions. For small manufacturers, it can mean bankruptcy.
What’s Changing in 2026
The industry is waking up. The ICH Q12 guideline, effective since late 2023, allows companies to make changes to manufacturing or packaging after approval - without restarting full stability studies - if they can prove it won’t affect safety. This encourages innovation. The FDA’s pilot program for continuous manufacturing is showing that shelf life can be determined 40% faster by monitoring product quality in real time, rather than waiting for batch results. And companies are finally investing in predictive models. The IQ Consortium’s Risk-Based Predictive Stability (RBPS) tools cut shelf-life determination time by 30% in trials with Amgen and Merck. But regulatory agencies still hesitate to accept them widely - because there’s no clear rulebook for what’s “scientifically justifiable.” Climate change is adding pressure. A 2022 MIT study projected that by 2050, rising warehouse temperatures could shorten average drug shelf life by nearly five months. In low-income countries, 28.7% of medicines fail stability tests because they’re stored in uncontrolled environments. In high-income countries, it’s just 1.2%.What You Can Do
If you’re a patient:- Don’t assume your medicine is safe just because the date hasn’t passed. If it smells odd, looks different, or feels gritty, don’t take it.
- Store medications in a cool, dry place - not the bathroom or car.
- If you’re on a critical medication like insulin, thyroid hormone, or seizure drugs, ask your pharmacist: “Is this generic version stable under my storage conditions?”
- Check for bulging cans, broken seals, or unusual odors - even if the date is far off.
- Refrigerated products like soups or sauces degrade faster if left out for more than two hours. Don’t rely on the date alone.
Final Thought
Stability isn’t a checkbox. It’s a continuous, science-driven commitment. For pharmaceuticals and food, shelf life isn’t just about when something expires - it’s about when it becomes unsafe. The systems in place are strong, but they’re only as good as the people who follow them. And the most vulnerable? The ones who don’t know to ask the questions.How long can I keep a generic drug after its expiration date?
You shouldn’t. Expiration dates are the last day the manufacturer guarantees the product’s full potency and safety. After that, chemical breakdown, microbial growth, or physical changes can occur. Some studies suggest certain pills may retain potency for years, but there’s no way to know for sure without lab testing. For critical medications - like heart drugs, insulin, or epinephrine - using expired versions can be life-threatening.
Are generic drugs less stable than brand-name ones?
Not always - but they can be. Generics must match the active ingredient and bioequivalence of the brand-name drug, but they often use different fillers, coatings, or packaging. These differences can affect how moisture, light, or heat impacts the drug. For example, a 2020 FDA study found some generic levothyroxine products degraded faster due to poorer moisture protection. Always store generics the same way you would brand-name drugs - in a cool, dry place.
What does ‘room temperature’ really mean for drug storage?
Regulators define it as 15-30°C (59-86°F), but stability studies use 24-25°C as the standard. Your bathroom or kitchen cabinet might hit 35°C in summer - especially in warm climates. That’s outside the approved range. For best results, store medications in a drawer or closet away from heat and humidity - not above the sink or near the stove.
Can I trust accelerated stability testing results?
Not entirely. Accelerated testing (40°C, 75% RH for 6 months) is used to predict long-term stability, but it can miss real-world degradation pathways. High heat can trigger chemical reactions that don’t happen at room temperature - or skip steps and create new harmful compounds. Many recalls have happened because accelerated tests showed no issues, but real-time studies revealed problems later. Always ask if the product has real-time data backing its shelf life.
Why do some food products last longer than others?
It depends on water activity (aw), pH, and preservatives. Low water activity (like in dried fruit or jerky) slows microbial growth. Acidic foods (like pickles or yogurt) naturally resist bacteria. Preservatives like sodium benzoate or potassium sorbate extend shelf life - but they can break down over time. Some companies use advanced monitoring of aw and pH to extend shelf life by 20% or more, but these aren’t always labeled. If a product claims “no preservatives,” it likely has a shorter shelf life.

Comments (9)