Vitamin K Intake Calculator
Vitamin K Intake Calculator
Calculate your daily vitamin K intake and see how it compares to your baseline. Consistent vitamin K intake is critical for stable INR levels while on warfarin.
Living with warfarin means you have to watch what lands on your plate. Even a tiny swing in your diet can push your INR out of the safe zone, and that can mean a clot or a bleed. This guide walks you through every food that matters, explains why it matters, and gives you a step‑by‑step plan to keep your INR steady.
What warfarin does - and why food matters
Warfarin is an oral anticoagulant that blocks the enzyme vitamin K epoxide reductase, stopping the activation of clotting factors II, VII, IX and X. By lowering the body’s ability to form clots, it protects people with atrial fibrillation, mechanical heart valves, deep‑vein thrombosis or pulmonary embolism from life‑threatening events.
Because warfarin’s effect hinges on vitamin K, any food that contains this vitamin can either blunt the drug (if you eat more) or boost it (if you eat less). The goal isn’t to ban green veggies; it’s to keep your vitamin K intake consistent day‑to‑day so your International Normalized Ratio (INR) stays in the therapeutic range.
Understanding INR and the therapeutic window
The INR is a blood test that measures how long it takes your blood to clot compared with a normal sample. Most patients aim for an INR of 2.0-3.0; mechanical mitral valves often need a tighter 2.5-3.5 range. Below 2.0 raises clot risk, above 3.0 raises bleeding risk. Small dietary changes can shift the INR by 0.5-1.0 units within a few days, so stability is key.
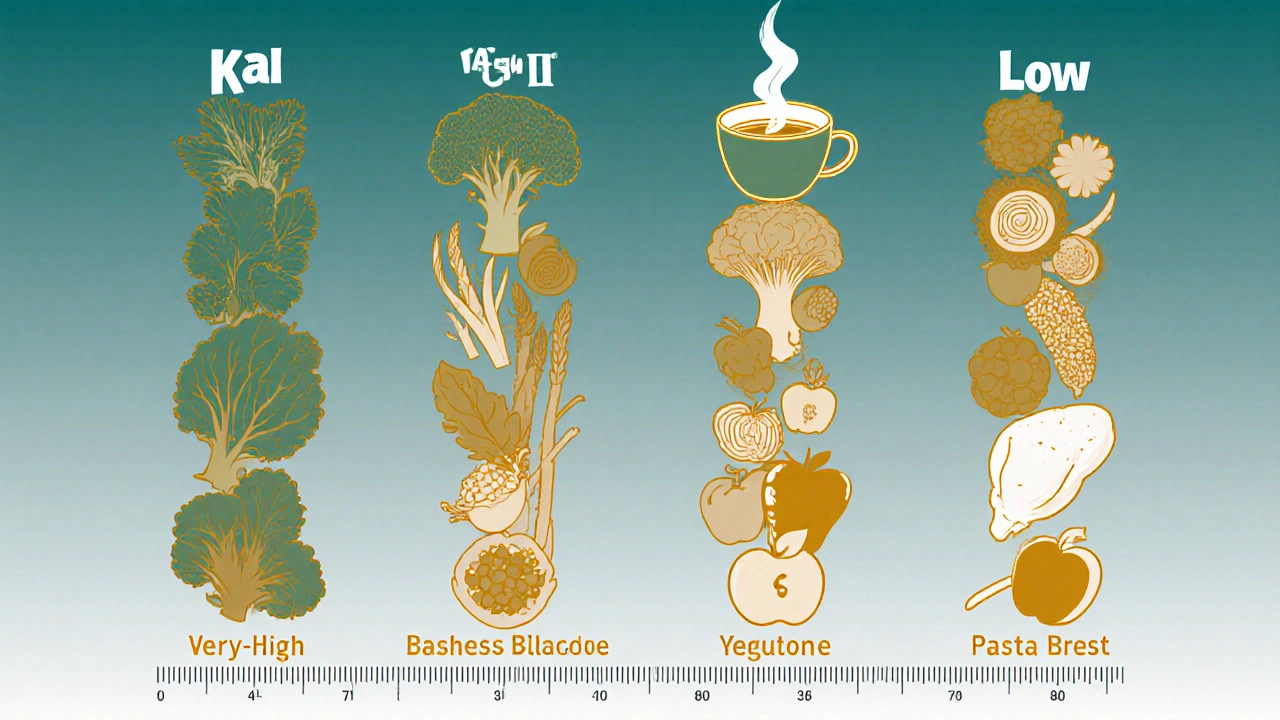
Complete food list - sorted by vitamin K content
Researchers at the British Columbia Ministry of Health grouped foods into three tiers. The numbers are per 100 g serving; remember that a “serving” on your plate may be larger or smaller.
| Category | Vitamin K (μg/100 g) | Typical examples |
|---|---|---|
| Very High | >500 | Kale (817), Collards (623), Parsley (616), Seaweed (599), Spinach (483), Swiss chard (450), Turnip greens (421) |
| High | 100‑500 | Broccoli (102), Brussels sprouts (177), Green tea (106) |
| Medium | 25‑100 | Asparagus (70), Cabbage (60), Lettuce (30) |
| Low | <25 | Apples, Berries, Rice, Pasta, Chicken breast |
Key take‑away: If you decide to eat kale three times a week, keep that schedule steady. Jump from zero to a bowl of kale one day and a bowl of lettuce the next, and your INR could swing by half a point in under a week.
Foods and drinks that do more than vitamin K
- Cranberry juice blocks the CYP2C9 enzyme that breaks down warfarin, often raising INR by 1‑2 units. Even an 8‑oz glass daily can push a 2.4 INR to 4.1 within a few days.
- Grapefruit juice inhibits CYP3A4, increasing bleeding risk by roughly 30%.
- Alcohol in excess (>3 drinks/day) cuts warfarin’s effect by 15‑20%; moderate use (≤2 drinks) is generally safe if spaced out.
All three should be avoided or used with strict medical guidance.
Supplements that can tip the scale
- Fish oil (omega‑3) - raises bleeding risk about 25%.
- Garlic capsules - can lift INR by 0.8‑1.2 units.
- Ginkgo biloba - linked to a 40% increase in bleeding events.
Before adding any over‑the‑counter product, talk to your anticoagulation clinic.
Practical guidelines for a stable INR
- Set a baseline: Record your usual weekly vitamin K intake for one month before starting warfarin. Use a food‑tracking app that flags vitamin K (MyFitnessPal, Cronometer).
- Stay consistent: Keep the amount of high‑K foods (like spinach or kale) within ±10% of your baseline every day. If you eat 1 cup of cooked spinach (≈889 μg) one day, try to match that amount daily.
- Avoid trigger drinks: No cranberry or grapefruit juice unless your doctor adjusts the dose.
- If you love tart flavor, switch to diluted pomegranate or plain water.
- Limit alcohol: No more than 2 standard drinks per day and at least two alcohol‑free days each week.
- Check supplements: Only take those approved by your pharmacist. Keep a list handy for each clinic visit.
- Schedule regular INR tests: Early in therapy, weekly tests are common; once stable, most clinics move to every 2-4 weeks.
Studies show patients who keep a food journal achieve a 22% lower rate of out‑of‑range INR readings.
Tools and resources
- WarfarinWise meal‑planning service - $49/month, provides portion‑controlled recipes.
- Vitamin K‑Controlled Meal Kits by Nutrisystem - each meal contains 25‑30 µg of vitamin K.
- WarfarinDoseIQ algorithm (FDA‑approved 2024) - integrates your logged intake to suggest dose tweaks.
All of these can be used alongside your clinic’s dosing guidelines.
Red flags - when to call your provider or go to the ER
Even with perfect diet control, warfarin can cause bleeding. Seek help immediately if you notice any of the following:
- Bleeding from a cut that lasts longer than 5 minutes.
- Black or bloody stools (possible GI bleed).
- Severe headache or sudden vision changes (risk of intracranial hemorrhage).
- Unexplained bruising or swelling.
These symptoms account for a sizable portion of warfarin‑related emergency visits, according to CDC data.
FAQ
Can I eat green vegetables while on warfarin?
Yes. The key is consistency. Pick a serving size you can eat every day and stick to it. Sudden increases or cuts can shift your INR.
How much cranberry juice is unsafe?
Even an 8‑ounce glass each day can raise INR by 1‑2 units. Most clinicians advise stopping it completely unless the dose is closely monitored.
What is a safe alcohol limit?
No more than two standard drinks per day, and at least two alcohol‑free days per week, keeps warfarin efficacy stable for most people.
Do fish oil supplements increase bleeding?
Yes, omega‑3s can raise bleeding risk by about 25%. Talk to your doctor before adding them.
How often should I get my INR checked?
During the first few weeks, weekly testing is common. Once stable, most patients move to every 2-4 weeks, depending on their clinic’s protocol.
Sticking to a consistent diet, avoiding high‑risk juices, and using reliable tracking tools make warfarin manageable. Remember, the goal isn’t restriction-it’s predictability.

Comments (8)