Medication Benefit-Risk Calculator
This tool helps you understand how healthcare providers weigh medication benefits against potential risks. Based on your inputs, it calculates a benefit-risk ratio to help you and your doctor discuss whether the drug's benefits outweigh the potential harms.
Note: This is for educational purposes only. Always consult your healthcare provider before making treatment decisions.
Enter Your Situation
Your Benefit-Risk Assessment
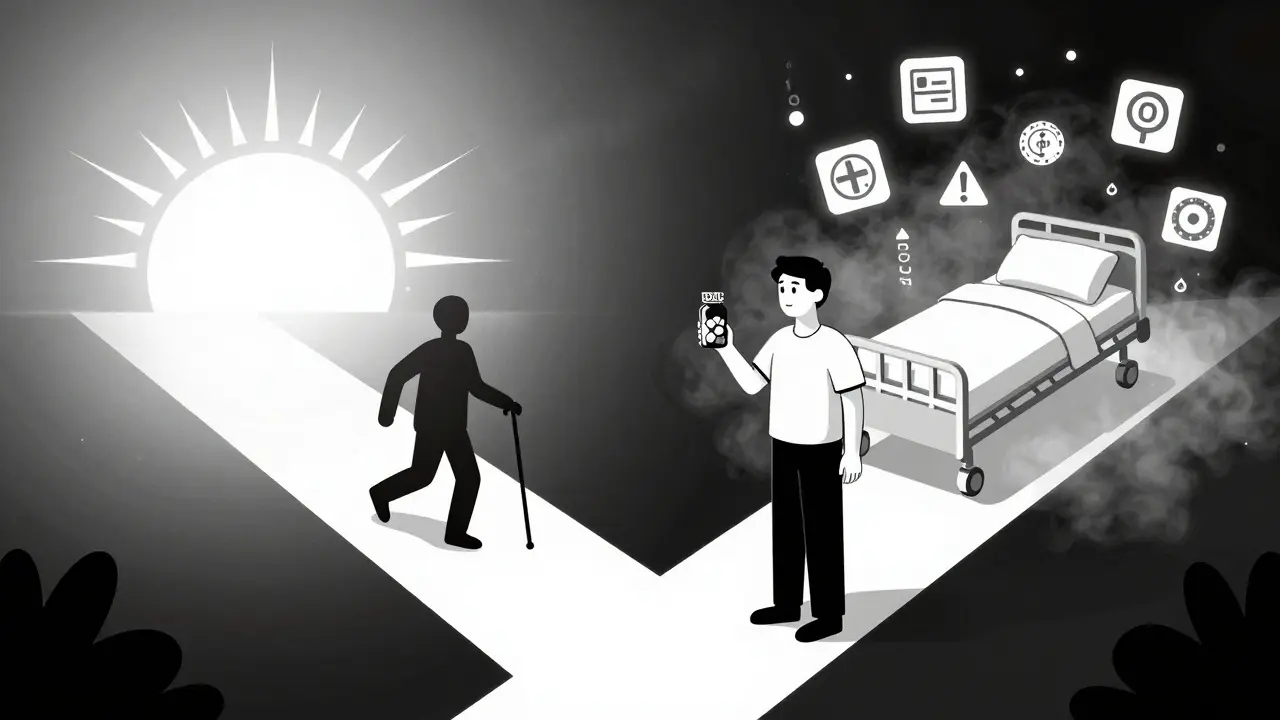
Every time a doctor prescribes a pill, they’re not just writing a script-they’re making a high-stakes call between healing and harm. It’s not about whether a drug works. It’s about whether the good it does is worth the damage it might cause. This isn’t guesswork. It’s a structured, science-backed process called benefit-risk assessment, and it’s the backbone of every medication decision in modern medicine.
What Exactly Is Benefit-Risk Assessment?
Benefit-risk assessment is how doctors and regulators decide if a drug’s positive effects outweigh its dangers. It’s not a simple checklist. It’s a deep dive into what the drug does, who it’s for, and what could go wrong. The U.S. Food and Drug Administration (FDA) built this system to make sure no drug reaches patients unless the benefits clearly beat the risks. That’s why, according to FDA Commissioner Robert M. Califf, a drug is only considered "safe" if its expected benefits are greater than its potential harms.This isn’t just theory. Every approved drug goes through this filter. Take Zolgensma, a gene therapy for spinal muscular atrophy. It costs $2.1 million and can cause serious liver damage. But for babies with this fatal condition, the alternative is paralysis and early death. So, despite the risks, it was approved. Why? Because the benefit-giving a child a chance to live-was far greater than the risk.
How Do Providers Actually Do This?
It starts with context. A drug that’s risky for a mild headache might be life-saving for a heart attack. Doctors look at four things:- The condition: Is it deadly? Chronic? Mild? A drug with a 15% chance of nausea might be fine for seasonal allergies but unacceptable for a patient with terminal cancer who’s already vomiting.
- Current options: Are there other drugs? Are they worse? If the only alternative is a 70% chance of stroke, a drug with a 5% risk of rash looks better.
- How well it works: Does it reduce tumor size by 70%? Cut stroke risk by 25%? Improve mobility? These numbers matter. A drug that helps 40% of patients with metastatic melanoma live five years or longer is a game-changer-even if 40% also get serious immune side effects.
- What can go wrong: How common are side effects? Are they temporary? Permanent? Deadly? A 0.1% risk of angioedema (swelling of the throat) sounds tiny, but for a patient with asthma, it’s terrifying.
Doctors don’t just rely on clinical trial data. They know real-world results are often 20-30% weaker than what’s reported. They also factor in how well patients stick to the treatment. If a drug causes constant fatigue, people stop taking it-and then it doesn’t work at all.
Why Patients and Doctors See Things Differently
Here’s where it gets messy. Patients and doctors don’t weigh risks the same way.Take hypertension. A doctor knows that ACE inhibitors cut stroke risk by 25%. But patients hear: "There’s a 1 in 1,000 chance you could swell up and stop breathing." That’s not a statistic-it’s a nightmare. A Reddit user shared how they refused the drug after reading about angioedema, even though their stroke risk was high. The doctor saw logic. The patient saw danger.
Studies show patients are often more willing to accept risk than clinicians think. In Parkinson’s disease, patients said they’d accept a 20% chance of involuntary movements if it meant a 30% improvement in walking. Doctors guessed they’d only tolerate 12%. In rare diseases, 78% of patients surveyed said they’d take higher risks than doctors recommended. Why? Because their daily reality is worse than the side effects.
Another example: Keytruda for melanoma. Oncologists explain: "40% of you will have serious immune side effects. But your five-year survival jumps from 10% to 35%." Most patients say yes. Not because they don’t fear side effects-but because they fear death more.
How the System Is Changing
The FDA didn’t always have this framework. It was formalized in 2013 and updated in 2021. Now, it’s not just about data-it’s about people. The 21st Century Cures Act (2016) forced regulators to listen to patients. They now survey thousands of people with rare diseases to understand what trade-offs they’d make.Tools like the FDA’s Patient Decision Aids-47 condition-specific guides-are helping patients understand risk. At Mayo Clinic and Johns Hopkins, these tools cut non-adherence by 22%. That’s huge. When patients truly understand the numbers, they’re more likely to stick with treatment.
AI is stepping in too. Top pharmaceutical companies now use machine learning to predict real-world side effects before a drug even hits the market. Roche’s ARIA platform cut prediction errors by 30%, helping them spot risks earlier.
Where the System Still Falls Short
Despite all this, big gaps remain.First, diversity. Clinical trials are still mostly white. A 2023 study found 75% of trial participants were White, even though minorities make up 40% of the U.S. population. That means we don’t know how some drugs affect Black, Hispanic, or Indigenous patients as well. A side effect that’s rare in one group might be common in another-and we won’t know until it’s too late.
Second, prevention drugs. The FDA hesitated to approve new heart disease drugs in 2022 because they increased bleeding risk. Even though they lowered heart attacks, the benefit didn’t outweigh the danger for healthy people. That’s the right call-but it leaves millions of people with borderline risk without options.
Third, cost. A drug can be perfectly safe and effective-but if it costs $500,000 a year, who gets it? The benefit-risk assessment doesn’t include price. But in real life, price decides access. A drug that saves lives might as well not exist if only the wealthy can afford it.

What This Means for You
If you’re taking a medication, don’t just accept the prescription. Ask: What’s the benefit? What’s the risk? And how does it compare to what I’m doing now?Don’t let fear stop you. But don’t ignore red flags either. If your doctor says, "This drug has a 1 in 10 chance of nausea," ask: "Is that 1 in 10 people, or 1 in 10 times I take it?" Most people misunderstand probability. Only 35% of patients correctly interpret "10% risk" as "1 in 10 chance," according to JAMA Internal Medicine.
Use the tools. The FDA has free decision aids for diabetes, depression, arthritis, and more. They’re designed to help you understand what you’re signing up for-not to scare you, but to empower you.
And remember: your values matter. If you’d rather live with pain than risk liver damage, say so. If you’d rather take a chance on a new drug than live with constant fatigue, tell your doctor. Your voice is part of the assessment now.
What’s Next?
By 2030, benefit-risk assessments will be personalized. Instead of "this drug helps 40% of people," you’ll hear: "This drug has a 68% chance of helping you, based on your genes, your weight, your liver function, and your lifestyle." That’s the future-and it’s coming fast.Right now, the system isn’t perfect. But it’s the best we have. And it’s getting better-not because regulators are smarter, but because patients are demanding to be heard.
Why do doctors prescribe drugs with serious side effects?
Doctors prescribe drugs with serious side effects when the alternative is worse. For example, chemotherapy causes nausea, hair loss, and fatigue-but for many cancers, it’s the only thing that stops the disease from killing the patient. The decision isn’t made lightly. It’s based on data showing the drug extends life, improves quality of life, or prevents a worse outcome. If the risk of not taking the drug is higher than the risk of taking it, the balance tips in favor of treatment.
Are all side effects listed on the label equally likely?
No. Drug labels list all side effects observed in clinical trials, even rare ones. But frequency matters. A side effect listed as "common" happens in more than 1 in 10 people. "Rare" means fewer than 1 in 1,000. Many patients panic reading a long list of side effects, but most are extremely unlikely. Always ask your doctor: "How common is this?" and "What’s the most serious risk?" That cuts through the noise.
Why do some people stop taking their meds even when they work?
Because side effects feel real, and benefits feel slow. A drug that lowers blood pressure by 10 points doesn’t make you feel better right away. But if it gives you a headache or makes you dizzy, you feel it immediately. That’s why adherence drops. Studies show 50% of patients stop taking chronic meds within a year-not because they’re noncompliant, but because the trade-off didn’t feel worth it. That’s why patient education and shared decision-making are critical.
Do generic drugs have the same benefit-risk profile as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name drug. They must also prove they work the same way in the body. The only differences are inactive ingredients (like fillers or dyes), which rarely affect safety or effectiveness. If you’ve had no issues with the brand, you can safely switch to the generic.
Can I trust what my doctor says about risks and benefits?
Mostly, yes-but don’t assume they know your personal risk tolerance. Doctors are trained in clinical data, not personal preferences. You’re the expert on your own life. If you’re afraid of a side effect, say so. If you’d rather avoid hospitalization even if it means taking more pills, tell them. The best decisions happen when your values and their expertise align.
How do new drugs get approved if we don’t know all the long-term risks?
Many drugs are approved under accelerated pathways, especially for life-threatening conditions. The FDA allows approval based on early data if the benefit is clear and the disease has no good alternatives. But that comes with a catch: the company must continue studying the drug after it’s on the market. This is called post-marketing surveillance. If new serious risks appear, the FDA can add warnings, restrict use, or even pull the drug. About 60% of drugs approved through accelerated pathways have incomplete long-term safety data at launch.

Comments (10)